The Doe’s Latest Stories

My Vaginismus Story: Understanding My Pap Smear Fear
I’ve avoided gynecologists for most of my life, but in the times that I’ve tried to overcome my fears and get a full examination, there was no way that cold speculum was going in. Until recently, I’d never experienced internal self-pleasure or penetration of any kind. It was only after my fifth try at penetrative sex that I realized my vagina wouldn’t allow anything inside. I didn’t understand what was wrong with me.
My Religious Upbringing Is a Contributor to My Vaginismus Symptoms
I’d been indoctrinated to believe that sex before marriage was a sin. I grew up in an Eastern Christian Orthodox family, one that was incredibly religious and my parents were really strict. When my father saw me hugging a male friend goodbye one day in high school, I received a huge lecture about not touching boys and that hugs were forbidden. In the years since leaving my parents’ home, I’ve become more progressive about everything, including sex, but my own relationship with it was the one thing I couldn’t let go of. I understood the limitations of my thinking around sex, how heteronormative it was and how patriarchal ideas like purity and virginity are. I became sex-positive for everyone else but not myself. It was too entrenched in my mind that if I did it, something terrible would happen. I couldn’t get the thought of my parents’ faces, my grandmother’s face, even my late grandfather’s face out of my head whenever the thought of it came to my mind. Like many other heterosexual Christian girls, I found the loopholes that eased my conscience. I engaged in other forms of sexual activity with long-term boyfriends but always drew the line at penetration. Although I still felt guilt, I managed to convince myself that at least I wasn’t crossing the ultimate line (even if my politics around sexuality told me otherwise).

I didn’t understand what was wrong with me.
I Experienced Vaginismus in My Marriage, Even Though I Felt Safe With My Husband
My boyfriend at the time didn’t have the same puritanical views on sex, but he understood what I needed and respected that. We were together for eight years before we got married. In that time, we got to know other aspects of our sexuality and intimacy that were fulfilling. Yet here I was, married and on my honeymoon, doing it with my husband, and something bad was happening. I hadn’t waited all this time to have sex just to continue not having it. I was in denial for a few months about what was happening. I thought if we tried enough, I’d get it right eventually. Sex became a high-pressure activity, one that I needed to overcome rather than enjoy. Sadly, in my mind at the time, all the creative and pleasurable ways we engaged in sexual intimacy before marriage became unimportant to me. I needed to get over the line for it to count.
I Was Unable to Do a Pap Smear With My Vaginismus, and My Doctor Further Traumatized Me
I didn’t know until after a visit to the gynecologist that I had a condition called vaginismus. Vaginismus is a condition that results in a trauma response to vaginal insertion of various kinds. It’s an automatic tightening of the vagina, one that you have no control over. Unfortunately, the doctor who diagnosed me wasn’t the best person to deliver that news. During our exam, I mentioned it was my first time seeing a gyno and that I’d waited for marriage to have sex, so I’d never done a Pap smear. “You did the right thing,” she said. That was the first red flag, but I just ignored it because I thought she was trying to be nice.I was convulsing and fighting as she held my legs open while she tried to insert the speculum. The gynecologist was visibly frustrated and warned me that I had to relax because she didn’t want to sexually assault me—not the best way to calm someone down. When my body refused, she gave up and sternly told me that I probably have sexual dysfunction. Ashamed and in shock, I put my clothes back on. I confided that I was having trouble with sex. She asked me if I had experienced any sexual trauma in my life. I hadn’t, at least not in the capital-T sense of Trauma, but the ways I was taught to associate sex with danger had traumatized me in more subtle ways. Then she told me that if I don’t work on this, my husband would leave me. I brushed this comment off because I knew better. I’d never let this kind of thinking get to me before. I was secure in a loving and dynamic relationship. I believed my pleasure was just as important as my husband’s, and I know that sex is more than just a penis penetrating a vagina. But hearing those damaging sentiments from a woman and her way of handling this very delicate situation was traumatizing. I walked out of there thinking I could never go back to a gynecologist again.
Ashamed and in shock, I put my clothes back on.
I Learned More Online and in Therapy About Vaginismus Than I Did From My Gynecologist
When I got home, I started Googling all the things I was experiencing and found a whole online community for vaginismus—the condition I now had a name for. Being able to name it was a relief, and finding out how many people around the world experience it made me feel so much less alone. If the gynecologist had been more informed about this, she could have helped me with information, different therapies and, more importantly, hope. Unfortunately, when I finally found the courage to go and see another doctor, she was just as ill-informed, and I felt like I was the one educating her during our consultation. Why would a whole medical specialty dedicated to helping women not be aware of something that causes so much physical and psychological pain for so many women?Luckily, I had the internet and a psychologist at the time. Through my online community and therapy, I’ve figured out that the way my community growing up handled the topic of sex was a form of trauma and that the boyfriends I’ve had along the way who pressured me into sex had only added to it. Dealing with the psychological side of the problem meant that I had to completely abandon the idea of penetrative sex and find pleasure in other kinds of sex again. Dilators have helped me ease the physical side somewhat, to the extent that I’ve managed to have a few pain-free and pleasurable experiences of penetration. Still, the thought of a Pap smear makes me anxious, and the worry that I may never be able to have one remains on my mind.
Confronting My Vaginismus Trauma and My Pap Smear Fear Head-On
Recently, I opened up to my GP about my condition. She’s kind and supportive in general, so it felt safe to tell her. She was sure she’d be able to work through it with me, and I felt hopeful. The next time I had a consultation, she told me we should give a Pap a try. Feeling relaxed and optimistic, I happily got on the bed and breathed deeply. As soon as the cold of the metal touched my vulva though, I seized up, and my legs immediately shut. My doctor was incredibly patient and tried to soothe me, breathing with me and gently trying to keep my legs open as she told me to put my hands on hers. Together, we approached my vulva again with the speculum. Again, every muscle on my body felt like it was contracting. I didn’t want to give up. We’d come this far, and I was so sure we were going to get it right this time. After about half an hour of trying, she told me we should quit and that she didn’t want to re-traumatize me. As soon as we stopped, tears came streaming down my face. I couldn’t stop crying. It was a shock reaction. I was embarrassed that I couldn’t control my emotions, but my doctor was as supportive as ever, and she helped me to calm down. “You haven’t failed,” she told me.

I Haven’t Completely Overcome Vaginismus, but I’m Not Alone in This Fight
I haven’t been back to try again, but now I'm more empowered than before. The internet once again helped me realize that I wasn’t alone. People have come up with their own therapies, bought their own speculums and developed whole programs to send to the doctor before a visit so that they can be informed about vaginismus. It’s quite amazing what people can do for each other, even with no formal organization or protocols. The field of medicine has always ignored women’s pain. They need to catch up to us now because we’re not waiting for them. Until then, I’m continuing to explore my body, find patience with it, heal my traumas and do what I can to break the cycle so that the next generation of young people can spread awareness, prevent and treat vaginismus.

I’m a Med School Dropout Turned Acupuncturist: My West-East Perspective
My personal struggles with physical and mental health took my lifelong dream and reshaped it into something I never could have imagined. Ever since I was little, I’ve wanted to be a doctor. My propensity for academia, curiosity with the human body and desire to be successful kept me on that path through high school and college, all the way to one of the top medical schools in the country. But it came with a price. I ended up in an environment that was so competitive that no one cared if I was even OK. It wasn’t until years later that I would find my true calling: acupuncture and traditional Chinese medicine. But luckily for me, none of my Western education has gone to waste, as the future is integrative medicine, and I am here for it.After graduating college with two degrees, working in an ER, doing research and crushing the MCAT, I was accepted to four amazing medical schools, and parts of my ego were at an all time high. I chose the California school for prestige and in-state tuition. But all the while, I was struggling with my mental health, so the competitive environment chewed me up and spat me out. My depression had gotten really bad after isolating to work on the applications, and my family situation was also very tumultuous, so I was feeling really unsupported and unprepared before school. I had a bad experience with a therapist/psychiatrist team that broke patient confidentiality with my family and misdiagnosed/mismedicated me. I sought solace and a sense of community in the rave culture and self-medicated with drugs and alcohol. But this just made things worse.By the time I got to medical school, I could barely focus enough to go to classes, so they started having me see the school psychologist and psychiatrist. They decided it would be in my best interest to go on medical leave of absence and return the following year. That meant leaving my on-campus housing, the only refuge from my toxic family environment, so it really didn’t do me any favors. I would drive down to school to continue seeing the therapist and the doctor, but my mental health just kept getting worse and worse.The therapist would listen to what I had to say but never really made any suggestions, goals or plans. He never recommended substance abuse treatment, group therapy or anything, really. The psychiatrist seemed burnt out and overworked, like he was bothered by the fact that he had to see me on top of all his other responsibilities. He didn’t think critically and went by the misdiagnosis from the previous practitioner. Even when I tried to explain why it was wrong, he didn’t listen. He didn’t care. They didn’t care about me, my progress or my success.
They didn’t care about me, my progress or my success.
I Found My Own Path Using Acupuncture and Eastern Medicine
I got tired of this and decided to forge my own path to feeling better. In the year that I had spent applying to medical school, I was starting to cultivate my spirituality via yoga and meditation, so once I left med school, I got a job at a yoga studio to stay busy and learn more about it. I practiced a lot and eventually did a 200-hour yoga teacher training. I started learning about spiritual practices, seeking something to help me manage my mood. I was introduced to Buddhism, which helped me raise my life condition and, I feel, led me to my current path: acupuncture. I wasn’t seeking acupuncture. To be honest, I had tried it a few times and been underwhelmed. But I was seeking a healer with some kind of ancient wisdom because I felt that would help me with my issues. I was still cycling through different psychologists and psychiatrists with little improvement. I was also having physical issues, like heartburn and chronic bladder irritation, that I needed help with. And last, but certainly not least, I needed to figure out what to do with my life. By this time, it was too late to go back to medical school, and I was working a dead-end desk job that I hated. Soon, I found an Ayurvedic (Indian traditional medicine) practitioner near my work who just happened to also be an acupuncturist. In our first session, this woman spent two hours with me and absolutely blew my mind. She got my entire physical and socio-emotional history and wove me a story about how the physical symptoms I was having were related to the emotions that I’d had because of the way I was raised. Everything was starting to make sense. Then she took me into the treatment room for a guided meditation, some acupuncture on my chakras, cupping, Thai massage and even some energy work. For the first time in a long time, I felt cared for.I felt like I could really open up to her, so I told her that I didn’t know what I wanted to do with my life. She asked what my background was, and I said medicine, and she literally said, “Why don’t you do this?” It was a lightbulb moment for me, and I left the office knowing I would study acupuncture. A few weeks later, I enrolled in acupuncture school, and five years later, I graduated and am preparing to get licensed. During the course of my education, I have witnessed and experienced numerous phenomena that are nothing short of miracles. A couple doses of herbs and an excruciating pain goes away. A few needles and a wonky digestive tract is fixed. Some energy work and months of anxiety and insomnia fade into a memory. I love what I do and the power it has given me to help others and myself.

Everything was starting to make sense.
Find Doctors and Practitioners That Actually Care for Your Health
So you’re probably thinking that I have sworn off Western medicine for acupuncture and Chinese medicine. But just like Western medicine, Eastern has its downfalls. I’ve spent hundreds of dollars on herbs and treatments that didn’t make any difference. I’ve gotten bruises from the needles or felt tired after treatments. One time, I was so out of it after acupuncture, I rear-ended someone. Another time, I gave myself a panic attack by taking herbs that interacted with a medication I was on. There were times when I was in a lot of pain and tried so desperately to only use natural methods to feel better with such little relief, but as soon as I caved and went the Western route, I felt so much better. While some practitioners, myself included, are very quick to refer to the Western doctors, I’ve had the other experience when I needed to be referred and wasn’t. Indeed, the downfalls of alternative practices are that they claim to heal everything. There are Eastern alternatives to things like antibiotics and antidepressants, but I believe it’s important to weigh the cost of these treatments and the ease of use when determining the best approach for an individual. If everyone had unlimited resources, we’d suggest acupuncture and herbs daily until they felt better, but all of my experiences have made me a realist and an advocate for an integrative approach. Especially when it comes to acute conditions—that’s where Western medicine really shines. Don’t deny yourself technology if you really need it. That is something I would like to change about the culture of alternative medicine and why I’m passionate about advocating for integrative medicine.As far as choosing practitioners, my takeaway is that there are incompetent, competent and exceptional practitioners in every field. There are providers that will help you and providers that will hurt you. I am by no means an expert in Eastern or Western medicine, but I’ve had a lot of experience as a patient of both. I’ve been saved by both and burned by both. The common thread was the doctors that cared who helped me the most. So when you’re looking for a practitioner of any modality, find the one who you feel like really cares, and that will make all the difference.

How I Overcame Yo-Yo Dieting and My Bad Relationship With Food
The first time I experienced body shaming was at a pool party when I was nine. I was wearing a new, hot pink one-piece bathing suit that my mother had bought when suddenly one of the boys splashed water my way and yelled, "Hey, Big Bird!" At first, I didn't understand the reference until he pointed to my stomach and said, "Skinny legs, fat stomach—just like Big Bird!" He squawked and flapped his arms before returning to a group of giggling kids by the pool steps. I glanced down at the wet, pink fabric that clung to my bulging stomach and was reminded of a brightly dyed Easter egg.Clinging to the rough edge of the concrete pool, I waited until the group of kids moved toward the diving board to make my escape from the water. Once inside the house, I quickly changed into dry clothes, then sat by the refreshment table where I stuffed fistfuls of potato chips into my mouth to numb the shame.I never wore that bathing suit again.My parents were always picky about my looks—they often poked my puffy belly to remind me I needed to stop snacking. I resented it but accepted it because I assumed it was their job to judge me. Weren't all parents concerned about their child's appearance? But being teased by my peers brought on a whole new level of shame that I was not emotionally equipped to handle.Around this time, I started really studying myself in the mirror (specifically the way my clothes fit) and rethinking my wardrobe. I hated that I was the tallest girl in my class, the last picked for relay race teams during recess and the first to rush home because I didn't want the boys yelling "Big Bird" or "Fatso" when I ran down the cracked sidewalk to my house.
I never wore that bathing suit again.
Yo-Yo Dieting Led to a Period of Disordered Eating
By the time I reached the sixth grade, I had begun the first of many diets. My sister and I did it together, counting every calorie we consumed and carefully measuring our food on a tiny kitchen scale. To my surprise, I quickly lost ten pounds, and the adrenaline rush I felt from my parent's compliments outweighed any cravings I might have had for junk food.But like many dieters, I found calorie counting too restrictive after a while and was quickly sucked into years of yo-yo dieting. As a result, my body became a human accordion; sometimes, I was thin, basking in the attention of high school boys. Other days, I felt fat and hid behind oversized clothing. The war with my body continued through my college years as I allowed the numbers on the bathroom scale to dictate my mindset. If the numbers were higher than I considered acceptable, I'd live on 600 calories a day. If I lost weight, I rewarded myself by binging on ice cream, hamburgers or whatever fried food I could get my hands on. It wasn't long before I discovered that I could eat as much as I wanted as long as I purged afterward.During this dangerous time, it never occurred to me that I was torturing my body in my quest to be thin, allowing this self-destructive behavior to continue for years until I finally met someone special and got married.
My Unhealthy Relationship With Food Resurfaced After Having Children
My husband was always generous with compliments, assuring me that I was beautiful and loved no matter what size I was. His easy acceptance of my appearance made me feel comfortable in my own skin for the first time since childhood. So instead of obsessing about my body, I focused my energy on starting a family and hit the gym regularly as a healthy alternative to control my weight.But nine years and four children later, the pounds crept back on. When I looked at my reflection, I hardly recognized myself. I thought the excess weight was muscle mass from my workouts. Still, there was no denying the swollen belly that triggered the same insecurities I felt at the elementary school pool party. Terrified of gaining more weight, I increased my cardio workouts and persuaded my doctor to prescribe weight loss medication. The drugs worked—I completely lost my appetite and dropped 40 pounds in two months.Certain my days of compulsive overeating were done, I reveled in my new smaller size and never tired of hearing people tell me I was getting too skinny or that I needed to gain a few pounds—this just fueled my desire to continue cutting more calories. Being thin was unchartered territory for me, opening new doors to a life I never knew existed. People smiled more at me, men flirted and women complimented my appearance. The anxiety I'd felt when I was overweight disappeared, replaced by a sense of confidence that I'd never experienced before. It didn't matter that the medication made me extraordinarily thin and jacked up my heart rate; all that mattered was that I looked skinny.

My Obsession With Body Image Rubbed Off on My Daughters
My obsession took its toll—the self-destructive cycle repeating itself in my daughters, who also had an unhealthy obsession with weight. As teenagers, they frequently examined their bodies in the mirror, tugged at their jeans and lamented the numbers on the scale. Their behavior reminded me so much of myself at that age, and I couldn't bear to think that they might spend the majority of their lives obsessing over their weight as I had. I felt as if I'd failed them by allowing them to grow up watching me criticize my appearance and for letting them see how my weight had defined me. I wanted them to focus on what was more important—their character and their health, and they needed to learn it from my example.I stopped cold turkey on the pills, and within weeks, my heart rate returned to normal as my weight increased. I tried not to panic when my clothes became a little snug, reminding myself it was best for my health.And it would have been if I hadn't let the old habits of compulsive eating creep back into my life.
I Became Naive About My Yo-Yo Weight Gain, and My Body Paid the Price
A series of events occurred that triggered me to numb my feelings with food. First, it was the grief of my mother's passing, which resulted in a falling out with my siblings. Then, I saw my son hospitalized for an addiction to nootropics. After that, I felt as if I was unraveling one pound at a time. In those four years, I gained 70 pounds and stopped caring how I looked. My life was in chaos, and the only solace I found was in the comforting arms of food.Despite the weight gain, I still embraced body positivity no matter how scary the escalating numbers were on the scale. I kept reminding myself that true beauty came from within and that it shouldn't matter how large or small I was, or what people thought of me, as long as I was happy with myself. So instead of staring at my expanding waistline in the mirror, I focused on the physical features that I felt were positive—good skin, nice eyes, a pretty mouth and a great smile. My mantra was, "If I feel good on the inside, then I'll look great on the outside!" But even though these words were repeated in my head daily, I was subconsciously disguising my body in larger clothing and avoiding full-length photos on social media.My body wasn't going to let me get away with that unrealistic way of thinking. It started first with my feet—they ached if I stood for too long during the day. Next, my doctor diagnosed plantar fasciitis and had me wear shoe inserts in addition to sleeping with special boots for my feet. After the foot pain subsided, I decided to exercise outdoors and trekked the mile trail near my house, only to limp back home after my left knee gave out.I was also exhausted all the time, falling asleep at my computer when I should have been working. The nights were worse—I couldn't get comfortable in bed because no matter what position I chose, the excess body weight pressed heavily on my chest, making it harder to breathe. My husband complained about the loud snoring and finally moved out of our bedroom and onto the couch. I thought of the people who used CPAP machines to help them sleep and vowed that would never be me—yet I continued to fool myself into thinking I was still at a normal weight. I believed that a few extra pounds wouldn't affect my health and that only people with morbid obesity had serious health issues. I wasn't at that point…yet…so why worry?

My Wake-Up Call to Break the Yo-Yo Diet Cycle
There were other problems occurring: A mammogram ordered by my doctor revealed two cysts inside my left breast. After doing a little research, I discovered that the statistics for breast cancer were higher for women my age who were overweight.More tests were ordered—blood work that indicated I was pre-diabetic and needed cholesterol medication. An inconclusive urine test required an ultrasound that later revealed that my gallbladder was loaded with stones—most likely from years of drinking alcohol and eating high-calorie foods.I woke one morning and stared at my puffy reflection in the mirror, no longer recognizing the dull-eyed, pasty-faced woman before me. Instead, what I saw was the face of my older sister, who had died years earlier from complications of her obesity.It was a moment of sudden clarity; my inability to face my obesity was costing me my health and leading me down the same destructive path that had taken my sister's life. It was the wake-up call I needed to change my unhealthy eating habits.
When I looked at my reflection, I hardly recognized myself.
I'm Finally Learning How to Have a Healthy Relationship With Food and My Body
Oddly, during the years I was thin, I suffered from body dysmorphic disorder, believing I was too fat despite being dangerously underweight. And then the reverse occurred once I became obese—there was a complete disconnect between myself and my body. As a result, I thought my weight was average and continued to give in to cravings for fattening, sugar-laden treats as a reward for my positivity.The only way to stop letting food control me was to think in terms of getting healthier, not "skinnier." I joined a popular weight-loss program that included a special meal plan and worked with a coach who helped me think of food more as a way to nourish my body rather than blocking unwanted emotions with large amounts of fattening snacks that did nothing to sustain me. Whenever I felt like straying from the plan, I called my coach or read inspirational stories on weight loss, which helped me to stay on track.I also joined a support group of people just like me with body image issues and eating disorders that helped give me the courage to stop my dependence on food for numbing myself. With support from family and close friends, I dropped the extra pounds in six months and no longer feared the allure of fattening foods. Instead, there was a sense of relief that was more freeing than the weight loss itself. By changing my life, I added more quality to it.I look better now, but more importantly, I feel better. The bodily aches, snoring, heartburn and pre-diabetic conditions have all disappeared with my weight loss. I am not too thin or overweight, but I am the best version of myself. I'm right where I need to be: healthier, stronger and happier—and currently the proud owner of a hot pink bathing suit.

My Endo Belly Is So Bloated I Look Pregnant
As society becomes more aware and accepting of the reasons why women can’t or don’t want to have children—whether for personal, political or environmental reasons—it’s become increasingly taboo to ask someone if they are pregnant. Still, in the past three months, I’ve been approached twice by people asking when I’m due.I’m not pregnant. I live with stage-four endometriosis, diagnosed through surgery earlier this year after ten years of extremely heavy periods and debilitating pain. It’s a full-body disease that is often misinterpreted and dismissed as “hormones” or “bad periods,” but its effects reach far wider than just bleeding. The most notable are reduced fertility and the inability to have children biologically. Endometriosis has been found on the lungs, brain and liver. In my case, they found extensive “deep infiltrating” cells growing in the lining of my stomach, which has contributed to intense gastric issues that were formerly misdiagnosed as IBS. A hallmark of both IBS and endometriosis is extreme bloating and swelling of the stomach caused by an inflamed abdomen, along with digestive issues that are intensified by the presence of the cells causing the enlarged stomach. Often it makes people with severe endometriosis look like we may be carrying a child.
I'm desperate for kids.
The Worst Part of My Endo Diagnosis Is That I May Not Be Able to Have My Own Children
Having my bloating mistaken for a baby bump has left me feeling ashamed about the way my body looks to others, but I’m more heartbroken by the knowledge that having a child of my own is a reality I will most likely never experience. I'm desperate for kids. I’ve always wanted tham, and I have a kind of innate feeling inside me that says I’d be good at mothering. I’ve worked with children in various capacities over the years, and whether teaching or nannying, I find caring for children to be incredibly fulfilling. Although I would happily have one of my own now, my partner and our current life setup say otherwise, but there is also the larger issue that I probably can’t have them anyway. During the operation where my endometriosis was diagnosed, the doctors also found a golf-ball-sized cyst on my ovary. Through sheer luck, and a lot of skill on the surgeon’s part, they removed it without having to take my ovary too. This is a rare occurrence in endo surgery, particularly if the operating team lacks specific experience, which is common. Endometriosis affects one in ten people who menstruate, but the number of patients far outweighs medical professionals trained in the specific treatments we need. In my surgery, they also found four centimeters of endometriosis covering my bowel. This was left untouched during surgery as a bowel specialist is required to be in the operating theater for its removal, as it’s deemed a higher-risk procedure. After coming round from surgery, high on IV morphine and still in excruciating pain, my surgeon showed me images of the inside of my womb covered in black speckles: the endometriosis. “It looks like your womb is inhospitable,” she said, “but there’s always IVF if you want to give pregnancy a go.” And with that, she was gone, leaving the images on my bedside table and wishing me a speedy recovery, saying we’d meet again to review in six months time.

Strangers Assuming My Endometriosis Belly Is Pregnancy Hurts Me Deeply
When the woman standing across the stall from me at the Saturday farmers' market asked if I was having a boy or a girl, I so badly wished I could say, “Yes, I can’t wait to meet my new daughter.” Instead, I felt my cheeks redden, my eyes cloud and my hands let go of the items I was going to purchase. I walked away clutching my boyfriend’s hand. I took to Instagram, tried to share the experience while veiling it in humor, to connect with other chronically ill friends who’ve had the same kind of interactions. I laughed about it and hoped my sadness would go away. But every night for the following week, as I drifted off to sleep at night, I thought of all the things I should have said to that woman and all the outfits I should wear to hide my bloating better. I read the statistics, looked up the cost of IVF and considered what I would do if I couldn’t make a child of my own. I’ve always been open to adoption, which aligns with the way I view the world. I grew up in an unconventional home, so I’m not adverse to making a family outside of the tradition.
Will I love my child the same if I can’t conceive her myself?
The Possibility of Not Being Able to Conceive My Own Child Haunts Me
It wasn’t until someone told me I probably cannot create a child the way most other couples do that I started to realize how much I wanted to experience pregnancy. I know, instinctually, I will love and mother any child I bring into my family, whether through adoption, birth or surrogacy, but it’s that intense feeling of growing another life inside me that I don’t think will be replicated any other way. For now, there is no baby in me—just a lot of gas and misplaced cells swelling my stomach to appear as if I am expecting. The people asking if I’m pregnant don’t know the pain I’m in or the string of questions I ask myself before I get to sleep every night: Will I love my child the same if I can’t conceive her myself? Will I be content? Will it ever be good enough?

The Body Positivity Movement Isn’t Just for Women
I consider myself to be a body-positive person. Gaining or losing a few pounds doesn’t really matter to me. Although I would be lying if I said it was something that I was born with—I had to learn it with the help of female empowerment and body-positive spaces online.After having my son in my mid-20s, I vowed to teach him what I had to learn on my own as a teenager: that his appearance was not representative of his value. That he’s much more than that. I felt even stronger about body acceptance now that I had a post-baby belly pooch and a few extra stretch marks. On the days that I struggled—on one occasion, feeling sad after a daring attempt to squeeze into an old pair of jeans—I found myself trawling the internet once again for feminist mantras, self-love quotes and pictures of normal female stomachs. Like a hug from an old friend, I was comforted.Something furious ignited within me as my son grew. I was determined to be a conscious parent, doing everything in my power to help my son to be a confident and self-assured kid in a world of Instagram, photoshop and body shame. On a warpath of empowerment, I armed myself with kids’ books about positive self-esteem and corrected myself when I used male-centric compliments, instead emphasizing his kindness rather than praising his tough exterior. I was learning. I still am now.Of course, despite my gentle push towards more neutral toys, he loved superheroes, so I indulged his interests and let him play with them, unaware that these buff characters would ultimately be damaging for his body image and contribute towards the narrative that men aren’t worthy or respected unless they are physically very fit.
What's missing is seeing real men's bodies rather than the sculpted, washboard, Greek-god abs in every movie and TV show.
My Son’s Superhero Toys Contribute to Toxic Masculinity
One day, he eyed the plastic lines etched into his action figure’s torso and asked me when a six-pack of his own would be appearing. At this moment, my heart broke. I knew that he was starting to think about his appearance and compare himself to the world. I didn’t want this to escalate into a deeper problem.I felt like I had failed as a mother. Where had I gone wrong?Naively, I had never viewed boys’ toys as problematic. Girls’ dolls are a different story, however, as the majority of us are familiar with how their tiny waists, breasts and heavy makeup teach girls to internalize this as ideal. On the other hand, superheroes and soldiers represent everything that men are told that they need to be—strong, infallible, a fixer of all problems. Essentially, a hero.It was like a lightbulb moment. “This is contributing toward toxic masculinity,” I thought. It didn’t feel right. Each action figure that my son owned had comically huge muscles, hyperrealistic bulging quads and vascular biceps, along with a sculpted six-pack. This is just as damaging as the girls’ dolls that parents tend to steer away from nowadays. In reality, a man would need a ridiculously low body fat percentage and a militant training regimen to maintain such a physique that these toys are perpetuating.

My Husband Got Hooked on His Body Image
I decided to do some research and found a worryingly empty space on the internet for men’s body positivity.Instead, it was disproportionately female, celebrating authentic bodies at unposed angles and the refreshing sight of unairbrushed skin. Lines, creases and stretch marks that felt as familiar as my own. I felt torn, as this female-led space helped me with my own body image issues, but I was powerless to change the fact that men’s normal flaws and diverse body types just don’t exist in the media.What's missing is seeing real men's bodies rather than the sculpted, washboard, Greek-god abs in every movie and TV show. The shirtless imagery that bombards us in every men’s lifestyle magazine.My motivations for a men’s body positivity movement weren’t just for my son. I had seen my husband struggle with his body image for years—at one point, his normal interest in working out spiraled into an obsession. I recognized my past self mirrored in him as he would pass by his reflection and pinch the tiniest amount of skin on his toned stomach. “I just need to get rid of this,” he would say, fiercely gripping anything he could around his torso.Helplessly, I watched as he would limit himself to just eating enough to meet his macros, some days drinking only protein shakes and exercising four, five, even six hours a day. My concern intensified as it escalated. I caught him taking dangerous fat-burning pills that he had secretly purchased from shady websites. Later, he confided in me that he was considering using steroids because, according to him, it was common amongst his friends.He was undeniably in amazing shape, but at the price of risking his health and falling into disordered eating behaviors, it was not worth the immense damage it was causing.

I couldn’t ignore that he was made to feel this way by society and the media.
We Need to Have More Conversations About Male Body Positivity
I couldn’t ignore that he was made to feel this way by society and the media.Men’s pressures to be ripped have been packaged as a fitness movement that is obtainable with normal gym habits. Actors and popular male fitness social media stars, who dedicate every waking moment to being in shape, often have personal chefs and trainers, and some use steroids to reach insane levels of being ripped very quickly. But they all declare that their muscular physique is the result of hard work and a good diet, which is highly problematic.My husband is now in recovery from his exercise addiction and complicated relationship with food. We tell our son that it’s OK if he wants to exercise when he’s older, that not everyone can get a six-pack. And that’s OK too. But more importantly, we emphasize the importance of practicing emotional honesty. While I can’t change the world alone, I can make small changes in my language and teach my son to be empowered and remain unphased by this outdated rhetoric, and encourage other men to share their stories.The facts are clear. Male body image needs to be discussed. Healthy doesn’t always look like a six-pack. Men are still valid and important if they’re not muscular. The notion of a “perfect physique” is not real.

My Mother’s Cancer Taught Me How to Navigate the Negative
It was the evening of October 27, 2020, when my phone rang. I was sitting in my college apartment in Gainesville, Florida, studying for midterms. On the other end of the line was my mother. I was expecting a catch-up call with my mom, but instead, my world stopped. Her words hit me like a freight train: “It’s cancer.” We cried, hung up, and then I cried some more. My mom—my best friend, my role model, my everything—had just been diagnosed with stage-three colon cancer, and I was hundreds of miles away. I’m the youngest of three—my two older brothers are my biggest blessings. My parents have always made sacrifices for us, and they have proven to me that love is unconditional. Thankfully, I grew up in a happy home. My family has always been there for each other, supporting each other's dreams, providing shoulders to cry on—we’re close. So that day, when I was receiving calls from my mom, dad, brothers and grandma, there were a lot of tears. We’re also a very strong, prideful family, so when I heard my favorite people crying on the phone, far away with nobody to hold, it was hard—quite possibly the hardest thing I’ve ever experienced.
Cancer dances between the lines of life and death but can also be used as a force to bring joy.
My Mom Is an Icon of Generosity
I’m fortunate enough to be able to say that life has not met me with much difficulty. I grew up in a loving home, made good grades, was involved in school, had friends and never felt the weight of deep sadness. This unfamiliar weight was so heavy on that day that the scale nearly broke. My mom, the most important woman in my life, had cancer and I couldn’t even hug her. On top of being so far away, we were in the middle of a global pandemic. With my mom being the genuine people-person that she is, it broke my heart to think she couldn’t see her friends or hug them—she couldn’t even leave the house. Despite the negatives stacked against her, she remained positive. My mom is the type of person who would wake up at 4 a.m. every day so she could prepare a fresh lunch for her kids to take to school, the one who cooks extra food for her coworkers. Upon walking through our front doors, she will always ask if you are hungry. (My friends have learned to arrive at our house with an empty stomach.) She hosted dinners for the cheer team, even after her daughter graduated. She always puts others before herself, and she is transparently honest. My mom is strong—the strongest woman I’ve ever met. Her motto is “Fighting!” because no matter what challenge she faces, she is prepared to fight through it and come out stronger—a quality that she has instilled in me. Now that she has cancer, the word “fighting!” gets thrown around like confetti. It may sound silly but hearing that word is what gets me through each day. Because we live in a small town, everyone knew about the cancer soon after the diagnosis. And since my mom is a pillar in our community and opens her kitchen and home to everyone, countless people wanted to help however they could. With so many people in her corner, my mom started to realize how loved she really is. As letters, flowers and meals poured in, my family grew even more thankful to have the life we do. Not only were we blessed to have our community in our corner, but we were blessed to have each other. In the process, we grew closer and stronger than ever before, which I didn’t think was possible. I am reluctant to admit that I have an unhealthy habit of avoiding my feelings. The support I experienced from my friends and family was nothing short of overwhelming. I’ve learned how important feelings and emotions are, and I have grown strong enough to recognize and appreciate my weaknesses. Despite my past tendency to avoid my feelings, my family held me while I let them pour—even hundreds of miles away.

I’ve Found Strength in My Mother’s Will to Fight
It’s interesting how cancer dances between the lines of life and death but can also be used as a force to bring joy. It has inadvertently strengthened me as a person, making me more genuine, hopeful and happy. I went home to see my mom the weekend after the doctors diagnosed her and surgically removed the tumor. I got there the day before she was released from the hospital. Physically, my mom was weak. Mentally, she stood strong. Although exhausted, she walked into our home with a big smile on her face, clearly ready to fight like hell. While every part of me wanted to stay home and be with my family, I knew I had to go back to school. Upon returning to Gainesville, a switch flipped. I studied more, became more organized and focused on the things I could control. Part of my drive was fueled by my attempt to avoid thinking about my mom’s diagnosis. But most of it came from my mom’s attitude about her diagnosis. She’s going through chemotherapy—currently in month four. Every day, she sends me a message with hearts, smiles, updates and of course, “Fighting!” Each day, she indirectly shows me her strength and drive to beat this thing. I do the same in return. In this way, my mom and I feed off of each other. That’s what keeps me going. I’ve learned that it’s okay to hurt and that you’re stronger than you think. I’m lucky to have the support system I do and to feel comfortable sharing these types of feelings. In the beginning, I was genuinely concerned that I wouldn’t be okay sitting in my apartment or do well in school. But here I am.
Not a day goes by that I’m not met with fear regarding my mom’s health.
Pain Can Be an Incredible Teacher
Through this experience, I’ve developed a healthy way to cope and navigate the challenges thrown in my life. A lot of it has to do with that amazing support system, but a lot of it also has to do with my strength. I used to be prideful yet humble. Now I’m confident and proud. I’m not conceited, but I would be a fool to dismiss my strength. As I allow myself to be strong and proud, I also give myself the time to mourn. I’m not saying any of this has been easy; I’m just saying it’s possible. Becoming a more positive person isn’t about always being happy. It’s about allowing room for hope. It’s not that the sun shines brighter now, but it’s the fact that I can see that one slim ray that makes it through on cloudy days. It’s not making myself smile more often; it’s finding more reasons to smile. It’s not about wanting to be cancer-free one day, but having the hope to fight until you are. To be positive is not to look at life through this lens that optimizes everything and everyone. Life throws us challenges. It’s unpredictable and oftentimes defeating. To be positive is to recognize reasons to keep going through these times—to have hope.Not a day goes by that I’m not met with fear regarding my mom’s health. I’m not saying there aren’t bad days because there are. On those days, you can hurt, and you can hurt as hard as you need. Through that hurt, you’ll start to realize the inner strength you didn’t know you had. You can use the negative to navigate your way to the positive. There can be good times, even during the bad times.

COVID-19 Has Been a Lifesaving Panacea for My Complex PTSD
I spent the first decade or so of my life fighting for my life. It’s shaped me in ways I am only now beginning to understand, and, oddly enough, I have COVID-19 to thank for this recent clarity.Enduring almost daily sessions of “percussive counseling” on the fists of my alcoholic father left a legacy that lingered long after the bruises faded. Friends and family members at the time noticed things were wrong early on, well before I had a clue that things weren’t right. What they didn’t realize in describing my behavior was that I was exhibiting traits not dissimilar to those of POWs after they returned from war. While other teens laughed and joked and rushed around me squealing with joy, I became shy and reclusive, apathetic on my good days, near numb or counterintuitively irritable and anxious on the not-so-good days.I was clearly exhibiting symptoms of what we now know to be complex PTSD.
Severe Childhood Trauma Has Shaped My Adult Behavior
Decades later, this unacknowledged and unresolved malady had deviously taken the driver’s seat in my life, and almost every aspect of my world suffered for it. Personal relationships never ran too deep, romantic relationships were doomed from the moment things became too personal and my personal relationship with truth and reality became tenuous at best. Why? Because when children experience severe trauma at the hands of their family, it creates confidence and trust issues that far too commonly last a lifetime. The reason for these issues is now well researched and understood; how can you ever trust another human being when the very people who brought you into the world didn’t love and protect you from themselves? Worse, you can’t help but ask yourself a soul-destroying question: What kind of piece of shit am I if the people who are supposed to love me unconditionally treat me like garbage? Learning to trust and be confident in one’s own inherent value are essential elements in early childhood, teenage and adult psychosocial development. If we can’t learn to trust people around us, or if we have zero confidence in our own personal value, and accordingly cannot trust our own capacity to build and live a meaningful life, then we are doomed—at least in part.For too many years, facing these questions head-on wasn’t an option, so I did what many of us do at times of existential angst: I buried my head in the sand. Over the years, I tried almost every known means of quieting the spiteful internal voices and ignoring the dull ache that comes with knowing you’re betraying yourself by hiding. When alcohol didn’t cut it, I turned to pills and powders. When those failed, I turned to my GP and began relying on pills that alternately had me experiencing vertigo or suicidal ideation, sometimes both. The cost of this period of my life—where I was, for all intents and purposes, a duck, calm on the surface but churning madly underwater—was tremendous. Outside of learning to rely on three to four hours of sleep and experiencing epic mood swings, it cost me a couple of high-paying jobs, some amazing friendships, a marriage and almost my life after a failed suicide attempt.Clearly, things had to change. In my case, it took a global pandemic to force my hand.
What kind of piece of shit am I if the people who are supposed to love me unconditionally treat me like garbage?
The Pandemic Offered a Shared Human Experience
When COVID-19 struck, I was working in Eastern Europe, thousands of miles away from home, from family and friends, basically as isolated as you could be. To say I hit rock bottom would be an understatement; I spiraled like Charlie Sheen in Vegas. So I booked a flight home. What I discovered upon returning home a handful of months into the pandemic was that people I had previously seen as standoffish or elitist were clamoring for human connection. Everywhere I looked, I could see clear signs of anxiety, uncertainty and social isolation. What I was witnessing was my own reality played out on a global scale; I realized that my harsh daily reality in which I felt anxious and isolated due to C-PTSD was now a common malady. Strangely, this made me feel the most human I had felt in years; I wasn’t so different after all.This recognition of a shared (albeit anxious) human experience started making me question how much of an actual victim I was allowing myself to be as a result of my childhood trauma and how much personal responsibility I was taking to change my own human experience. A chance encounter with a genuine asshole forced me to ponder—if my indignant next-door neighbor could so swiftly become affable (if not entirely likable) in such a short period of time due to his social isolation and a deep-seated need for human connection, what possibilities were open to me for taking responsibility for shifting my narrative from victim to victor?What I’ve come to understand through forced lockdowns, remote working and a liberal amount of “me time” is that there is potentially a very real upside to COVID-19. The global pandemic presents us with a deeply personal moment in time to reflect, reassess and start to take responsibility for “the me I want to be” on the other side of this mess.

I spiraled like Charlie Sheen in Vegas.
I Began to Look at My Health From a Holistic Perspective
The first penny that dropped for me when forced to reevaluate my life (which included realizing that I was, in part, my own worst enemy) was that I wasn’t a happy or healthy person when I entered the COVID-19 pandemic. I dearly wanted to change this before I came out the other side. Central to this clarity was recognizing that I had never taken the responsibility to think about what a healthy life could look like because I was in victim mode.As a lifelong runner, I have always somewhat shortsightedly viewed my health through the lens of “physical” health, yet this “hurry up and stop” moment in history that we find ourselves in has forced me to take a wider, more holistic view of health to encompass other aligned aspects such as my emotional, social, spiritual and intellectual health and wellness.This shift in focus—this widening of my worldview as it pertains to health —has resulted in an astonishingly rapid shift in my priorities and day-to-day realities. Emotionally speaking, I’m more stable than I’ve ever been because I have accepted that only I can take responsibility for this next chapter of my life, and as such, I need to do more of what really matters to me.From a social health perspective, I’ve become conscious of the five people I spend most of my time with, even in lockdown. This has included me moving back into university studies to fulfill a lifelong dream of completing a doctorate degree in a field that will have a genuine social impact. From a purely physical health standpoint, I’ve started being more responsible for what I eat, for what media I consume and for how much time I spend outdoors exercising. All of this has led to a drop of 15 pounds, a gradual increase in the duration and quality of my sleep and a greater connection with my partner now that I’m calmer, living more purposefully and more present.

COVID-19 Has Given Me a Chance at Salvation
I will be brutally honest—deep introspection hasn’t been easy. It’s been far more confronting and oftentimes more unnerving than I ever could have imagined. But it’s made easier by understanding that I’m not so very different from other people. We are all anxious, alone and uncertain at times, which has in an odd way given me the confidence to keep peeking behind the curtain and continue to pick at scabs that I had previously done my utmost to ignore. The pandemic has reshaped the world in many ways that we would prefer not to have happened, but for me, it’s also provided a rare opportunity to slow down and take a good hard look at my life, my health and wellness and to start making changes. And as I continue to see the fruits of my labor, to experience the results of taking responsibility and positive forward action, my self-confidence is improving, which helps me build trust in myself and the world around me.COVID-19 isn’t going away anytime soon; neither is my C-PTSD. But amid all the uncertainty that surrounds us, I have more confidence that COVID is my moment of salvation rather than a harbinger of doom after seeing the results of the responsible changes I have made.

What It's Been Like Living With a Binge Eating Disorder All of My Life
I am in recovery from binge eating disorder and compulsive eating, something that has given me a lot of demoralizing experiences and which has touched every area of my life: my body, mind, sexuality, emotions and spirit. As a kid, food was my greatest escape from dealing with my dysfunctional alcoholic family. As early as the second grade, I was stealing and hiding food, and I can still remember the shame that comes from it. We were at my grandmother’s house, and I was eyeing the cake on the table. I had already had a piece, and my mom told me, “No more.” So when she wasn’t looking, I cut a piece and ran to the bathroom upstairs. I heard my mom coming, and I hid the cake behind the toilet on the bare floor. My mom found it, looked at me and asked, “What’s this?” I had no answer. I just told her, “I don’t know,” while inside I was embarrassed and totally ashamed. I got a lot better at hiding it after that, but I wasn’t really hiding any of it. My body continued to be the most obvious symptom of my compulsive eating.
Over the course of my four years in college, I gained over 160 pounds.
My Attempt at Coping With Binge Eating Wasn’t Any Better Than Binge Eating Itself
Later on, in high school, I wanted a change. I got a personal trainer and went on a super restrictive diet. When I came back from summer break, it was dramatic, like one of those teen movies. I was suddenly “hot.” Girls wanted to date me, and everyone told me how amazing I looked. I allowed the joy to overshadow what I was actually experiencing. With my new weight and my new looks, people treated me differently. I thought perhaps it was because I was treating myself differently. But “pretty privilege” and fatphobia are a real thing. So is the insanity that comes with trying to keep this “privilege.” What no one knew was that I was chewing and spitting my food out, exercising three hours a day and binging on bread before heading to the gym. I got a girlfriend, and it looked like I was having an amazing high school experience. In many respects, I was. And then it ended. Between the stress of starting college, a breakup and my ongoing family issues, I just couldn’t control it anymore. I started to binge again. Violently. Consistently. All the time. Over the course of my four years in college, I gained over 160 pounds, and I became addicted to pornography.This time in my life was such a blur. I walked around every day feeling ashamed that I couldn’t control my compulsive eating. I was obsessed with food and obsessed with my weight. As much as I wanted to lose weight, I didn’t have the willpower to stop my compulsive eating. During this period in my life, I really struggled with my masculinity, my manhood and my connection to my sexuality. Firstly, as a man, I thought I should be able to control my eating, that I shouldn’t be powerless over something so simple. As men, we don’t talk enough about the mind-body connection and the deep need for men to feel connected to their body. My frame was obviously not that of a “normal” sized man, and I certainly didn’t feel like any woman would be attracted to me. I objectified my own body by picking it to pieces and body shaming myself day in and out.So I shut my heart and my body down. While I was a compulsive eater, I was also a sexual and emotional anorexic, starving myself of some of the basic human experiences any young man can have that allow him to grow and explore who he is in the world. No one talks about this, but imagine the effects when you can’t see your own privates when you look down because of your stomach. We all deserve freedom from shame and a level of safety to explore ourselves with others in this world. When you are the one that shuts this down for yourself, you deny yourself the dignity of your own experience. You feel like less of a man, less of a person and less deserving of love. After college, I moved to Los Angeles, where I immediately hit rock bottom. I was choosing food over shelter. I reached a point where I was living in a hotel room and using the last hundred dollars on my credit card to binge. I would go to CityWalk, the downtown restaurant district outside Universal Studios, bouncing from restaurant to restaurant to food stand. Or I would go from one drive-thru fast-food restaurant to another. The food didn’t taste good, but it wasn’t about the food—it was about not feeling. I knew I couldn’t do it anymore. I didn’t want to kill myself, but I finally knew that I couldn’t use food to push down all the unmanageability in my life. I wanted to cut myself rather than feel the pain that I had never really learned to cope with.

Confronting My Overeating Coping Mechanism and Healing From Binge Eating Disorder
Growing up, my father had found recovery in Alcoholics Anonymous, so I was familiar with the concept. I was randomly getting lunch with a friend when she shared with me a little bit about her recovery as an alcoholic. I don’t know how, or why, but I started to consider that maybe there was a program for me. I looked up Overeaters Anonymous and called the contact for a meeting. A stranger answered, and I told them I needed a meeting. I asked if I needed to bring anything. She said, “Just know you are giving yourself the greatest gift you could ever give yourself.” I went to a meeting and started my recovery journey. I found a new home in Overeaters Anonymous.Through this journey, I lost over 160 pounds, and I’ve maintained a healthy weight for over 14 years now. Compulsive eating and recovery are no joke. It takes a lot of work on a daily basis that I have to continue to be honest about. Between being in a 12-step program, therapy and everyday life, I am confronted with the reasons I ate on a daily basis. They say if you want to know why you’re compulsively eating, stop compulsively eating. So I did. I’ve had to heal from all the resentments and hurts I’ve obtained over the years, all the hurts I stuffed with food. I had to allow them to come to the surface and grieve. I’ve had to allow myself to grieve. I’m 38 now, but at times, I’m still in many ways a 16-year-old with a lot of unmanageable feelings.As a result of this healing, I also found my way into Sex and Love Addicts Anonymous. I’ve had to look at my addiction to pornography and my struggle to feel intimate and safe with the opposite sex. Today, I am a vulnerable, honest man who lives with integrity and grace. I do it very awkwardly and very clumsily. But I do it, and it’s imperfect.
It wasn’t about the food—it was about not feeling.
How to Deal With Binge Eating Disorder Varies From Person to Person
Through all these experiences, I found myself becoming an advocate for those in recovery from eating disorders, specifically men and people from marginalized communities. In eating disorder recovery, we all come in many different sizes and experiences. For some, we need to eat more. For some, we need to eat less. Our bodies might be a symptom of our eating disorder whether we are extremely overweight or underweight. Our needs are different, and we need to make room for all the narratives.We live in a world that glorifies health and wellness in a way that for many is unattainable. And let’s be honest, privilege, race, gender, sexuality and economics all play a part in one’s ability to reach those perceived goals. But now we are seeing a beautiful counterculture develop that’s pushing back. We have the body positivity movement, the fight against fatphobia and new medical perspectives that say people can be healthy at any size. However, even in this counterculture, I have struggled to find my place and my story within the recovery community. Binge eating disorder was only recognized as an actual eating disorder when it was added to the DSM-5 in 2013. I believe we are only now starting to understand the experience.

Overeating and Eating Disorders Are About Much More Than Body Positivity
I have issues with some of the ways we’re approaching healing from eating disorders though. In my advocacy work, I’ve been told that I can’t talk about my weight loss. Or if I do, that I can only talk about it very vaguely, in order not to trigger other people. When I was at my heaviest and seeking help, I needed to know that weight loss was possible. I felt trapped in my own body, and I didn’t understand that it was manifesting the symptoms of my compulsive eating. I thought I was just a failure with a weight problem. But when people shared their experiences with me, I knew I wasn’t alone.The truth is, body positivity alone isn’t eating disorder recovery. Wanting to lose weight does not make you fatphobic, and each individual has a right to decide what role “health” is going to play in their lives. As a compulsive eater, my biggest flaw was my people-pleasing. I stuffed my feelings because I just wanted to be loved, because I didn’t love myself. And even in recovery, I can find ways to beat the shit out of myself. So I’m letting it all go. Appearing healthy is so much more than my looks or my blood pressure. Where am I mentally, emotionally, spiritually? Be willing to define that truth for yourself, and be honest about whether it is working for you. I don’t subscribe to body positivity for myself. I prefer body neutrality. I’m not always going to feel good in my body, and that’s OK. Those feelings allow me to connect to other issues that might be going on. My body and my desire to stay at a weight that feels comfortable for me does not make me fatphobic. It just means I’m having my own experience.We live in a culture that constantly promises the next big thing, whether it’s diet culture or even recovery culture. But I’m telling you, the next big thing is when you say “fuck it” and define what’s best for you yourself. What brings you peace? What keeps you balanced? What allows you to connect with you? That’s an obsession I’ll stick with—because everything else is just a distraction.

My Father's Blindness Has Changed My Perspective on Life
As I awaken each morning, my eyes open to a blurry view. The softened edges of my surroundings are washed with unfocused light. I take a moment to lay in the fuzziness before I reach for my glasses and begin the day. No matter what state I am in, in the morning—perky, lethargic, hungover—that moment humbles me. Like many, I have myopia—a vision disorder known as nearsightedness. The blurriness reminds me of how easy it is to be debilitated. Myopia, of course, is a widespread disorder. Millions of people have some degree of nearsightedness, donning glasses or contact lenses each day in order to interact with the world. Often passed down through some combination of mutated genetics, it tends to affect many members of a family at some point in their lives. This is true for me and my family, our conditions ranging from common to high-degree. While the rest of us have easily addressed it, my dad’s case is more complex. Through an extensive traumatic period, he became irreversibly blind, his journey telling a story of lost vision and hard lessons.
My Father’s Transition to Living Blind
My father’s visual deficiency stretches back to his childhood. During his teenage years, he wore thick-rimmed glasses, their round, heavy frame pressing into his nose bridge. Without them, he couldn’t focus on anything beyond a few inches from his face. He wanted, like most of us, to restore his sight. In 1995, he underwent corrective eye surgery to reshape his cornea. At first, it was successful; his myopia was effectively treated. But his underlying glaucoma, unbeknownst to all until after the recovery process, worsened. A long string of rescue and additional corrective surgeries followed, creating an archive of scars and recoveries. Ultimately, this turbulent course ended in 2010—he was officially blind. The intervening steps were not enough to correct this trajectory. Over time, his sight diminished until only a generic gray remained, like the uncolored slush of snow eroded by traveling footsteps. He has recounted this story to me several times, inflected with a tone of regret. He usually speaks with a matter-of-fact tone, but occasionally, a wistful sigh escapes. When he does, he’ll linger most on his initial decision to undergo surgery. Should I have done this at all, he poses as I listen quietly. Where did I go wrong? If either of my siblings or I mention laser eye surgery, he bristles, affixing his adverse result on us like a warning label. Scarred by his own harm, he protests in order to protect despite how safe the procedure is today. In his time, it carried higher risk; now, it is commonplace.
He refuses to let his blindness define him.
My Family and I Took on New Roles to Help My Dad
Soon after his becoming blind, my family and I adapted the home to be more blind-friendly. We organized our efforts around my father’s memory of the layout, like decluttering the common hallways and strictly organizing the kitchen. I was encouraged to see how he could maintain some agency when moving about, borne of years of lived experience. (This is why we can stumble, drunk with sleep, to the bathroom at night without a second thought.) But despite his intrinsic map, he still needed to form new habits. A toothbrush had to be placed in a specific direction; freshly washed dishes were arranged in the drying rack to avoid sharp edges; paper bills were folded based on their denomination. These measures represented his pragmatic approach, a means to an end no matter the difficulty. With the private interior under our control, the public exterior—unpredictable and irregular—was next. I became hyper-aware of every step or slope; any obstacle on the ground, like an errant rock or uprooted piece of sidewalk, that I would otherwise avoid without a thought became a potential tripping hazard. When we would walk together, I would guide my dad, acting as his eyes. Instead of watching distant buildings, I focused on the immediate ground before us. Occasionally, I would say, “Step up on this curb,” or, “The next set of stairs has five steps,”—moving through space was reduced to mechanical instructions. Now living away from my parents, I notice any manhole that is slightly ajar, a loose cobblestone or a sidewalk curb whose delaminated steel face juts out—urban dangers that remain as visual texture for most. Whenever I visit home, I resume the same role, guiding with my eyes cast downward, his inward. He refuses to let his blindness define him. Ever practical, my father still works as a physician while blind, albeit at a slower and more intentional pace. Guided by routine, he implemented workarounds like training his short-term memory and delegating more on others. He listens and memorizes each appointment and dictates key points back to his assistants to record. He had to adapt and quickly, for there was still work to be done. When I can, I aid in quotidian tasks like checking and reading aloud emails and reviewing recent financial activities. These seemingly benign new roles became portals to parts of him that I would not otherwise directly encounter. Relaying aloud each month’s gain or loss, a newly incurred debt or an email bearing a difficult subject were often uncomfortable exposures—news that we learned together in real time. It dissolved the mirage of the fortified parent and instead laid bare his vulnerability

I Learned the Value of Physical and Emotional Touch
I quickly learned how physical, for my dad, things became. The textures of everyday objects became apparent, his hands taking the place of his eyes. Each time we go grocery shopping, he handles the cart, and I will pass him various foods for him to handle and evaluate. I know he was never a big shopping enthusiast, but I want him to be engaged. This apple is too soft, he will say. This egg is cracked; go get another carton. When we pay and leave the store, he will insist on carrying the bulk of the weight, partly out of desire to help but also, I suspect, to occupy his hands. These handy tasks were a way to keep nimble, exercising his other senses when one was lost. But the most intimate form of this physicality was his grip on my arm when walking. This grip could take on different configurations: a solid, clamped hand; a few loose fingers; linked elbows; a clasp on my shoulder. In one touch, I would try to detect his overall mood—a firm hold could indicate nervousness or unfamiliarity, a loose one could mean comfort or aloofness. If it was cold and windy out, he might extend his hand into a pocket and we would essentially hold elbows. I felt these moments were glimpses into his mind that would otherwise go unnoticed—so much of what we emote in a day goes unspoken. While these micromoods were minute, I felt more closely connected to the thoughts lingering behind his visage. Now whenever I see him, I notice his gestures more and study his face longer, yearning to learn from this wordless language. In December 2020, we were walking to a restaurant for dinner. While my parents had been before, this was my first time. Approaching an intersection, I pulled myself forward, planning to cross the street. The closer I got, the harder my dad pulled back. I urged him to come with me, but he wouldn’t budge. Finally, when the light turned red, his grip softened. Frustrated, I turned to face him. The restaurant is on this side of the street, he said and led us in the right direction. Despite the darkness, his inner compass still points north.
Despite the darkness, his inner compass still points north.
I Started to Become More Present and Mindful
Being the son of a blind father has been and continues to be a lifelong lesson. It inspired me to learn about and advocate for disability rights. Tactility and materiality are important components of my professional work as an architect, where I create space for others. I have learned to not only see things more intently but also to listen closely, smell acutely and taste fully. How I take in the surrounding world is influenced by both his blindness and my own desire to consume everything in case I suffer the same fate. I am nourished by the tinge of orange zest, the crusted faces of old brick and the faint sweetness of a springtime wind. I am driven to feel whole through all my senses in fear of losing one. Now every morning when I awake, I embrace the blurriness. The haze is comforting, a respite from the hyperrealism of corrected vision. It soothes the mind to pull back from hard lines and sharp edges and instead wade in a soup of light and shadow. By focusing on this softness, I go about my day with clear sight and intention. But by the end, I anticipate returning to the blurriness, like a sun setting beyond the horizon, out of sight.

I Was Staunchly Pro-Choice. I Was Shocked When My Abortion Was Devastating
When I was 28, I had an abortion at eight weeks pregnant. It was going smoothly. When the doctor at the Santa Cruz, California, Planned Parenthood said, “Now just isn’t the right time for this spirit to come to Earth,” I shrugged in response, feeling uncomfortable. She seemed to be trying to comfort me.“I don’t think of it that way,” I said. “It’s just a ball of cells.” I’d always defended the right to abortion with a “no big deal” attitude—having an abortion wasn’t anything other than a safe medical procedure. This abortion was no different. It was the logical choice given my rocky romantic relationship. I didn’t think of the embryo as a human life. And I had no second thoughts based on how the abortion would impact me in the future. In other words, the idea that abortion was “no big deal” wasn’t just a political stance—it was something I believed through and through.I projected this view onto others too. I sincerely thought that no one, save for those indoctrinated by religious, pro-life values, had any reason to experience complicated emotions around abortion. When the young woman next to me in the recovery area of Planned Parenthood was gushing tears, I silently judged her. Why would she be upset about terminating an unplanned pregnancy? If she decided she wanted a baby, then she could have one later—once she’d thought it through a bit more. But an unplanned pregnancy would ruin her life. Buck up, dear girl!
I. Just. Needed. A. Baby.
I Suffered From Post-Abortion Stress Syndrome
That’s where I stood before things got weird and my world turned upside down. About one year after the abortion, I went from my normal, friendly, punk-rock self to having bouts of extreme jealousy of pregnant women and women with children. I seethed at baby strollers. I also despaired that I was likely infertile (with no evidence to support this), and I suddenly felt the need to name the baby I’d lost—the one who used to be “a ball of cells.” In fact, I couldn’t think about anything but this baby. Months into this surreal turn, I learned these feelings might all be grouped under something called post-abortion stress syndrome, or PASS, for short. PASS is a condition in which you have some variety of negative feelings—often of regret or guilt—after an abortion. Pro-choice scholars usually claim that the condition is entirely fabricated. Anti-abortionists usually claim that it affects a large proportion of women who get abortions. I had never even heard of PASS before I started feeling this way. I thought I might be losing my mind until I found a non-religious, apolitical support community of women online who had experienced PASS. But my experience with PASS, and in the PASS support group, turned my world upside down in another way, too. I now had to believe that abortion could have an emotional, or perhaps even biopsychological, impact on at least some women. Because I was one of them. And, thus, my "no big deal" dogma began to crumble.As part of my experience of PASS, I had something we in the support group called “replacement baby syndrome.” I. Just. Needed. A. Baby. It would be like bringing my lost baby back to life. In fact, I wanted this baby so much that I could no longer picture using any birth control more premeditated than a condom. My last relationship had ended, and while I didn’t want to mingle bodily fluids with just any guy I slept with, I also didn’t want to make 100 percent certain that pregnancy didn’t happen. What if my date and I decided to procreate in the heat of the moment? The best way to leave that door open was to avoid highly effective, long-term birth control options like an IUD.

Planned Parenthood Made Me Feel Excluded in My Path to Motherhood
My resistance to formal birth control is how I found myself, at age 29, arguing with my Planned Parenthood physician. I had moved to Oakland, California, and taken the train north to the clinic.“So, it says here you are not using a regular birth control method,” she said. “We should talk about that.”“I don’t want to talk about it. I’m almost 30 years old, and I want to be a mother. I wrote that on my intake form,” I replied.“Well, being a parent is harder than you think,” said the young doctor. “I don’t care if it’s hard,” I’d said. That’s when the tears began brimming. “You’re just saying this because I’m single and working class. You don’t think I should have a baby in my position. I told you before, I don’t want to talk about birth control. I came in for a pelvic exam!”I burst into tears, asked her to leave and proceeded to hyperventilate alone in the exam room.I know that plenty of Planned Parenthood doctors would have respected my wishes to focus only on the health of my vagina during the exam and not my reproductive capacities. Perhaps some would have given me information about local fertility clinics or “single mom by choice” groups so I could pursue parenthood safely. Others might have recognized that I wasn’t in a great emotional place to have a baby but might have referred me for therapy to discuss my options. But that isn’t what happened, and I was starting to feel that there was no place for me in the pro-choice movement anymore. I began regularly venting to my friends about the eugenic history of Planned Parenthood and the failures of the movement to acknowledge PASS or accept unconventional paths toward parenthood.

I suggest naming this new stance 'pro-option.'
It’s Time to Move on From the Pro-Choice Movement and Start Being Pro-Option
Eleven years later, I no longer have PASS—mourning for my loss is now a distant memory. My frustrations with Planned Parenthood have long since been outweighed by the essential services they provide. I actually did end up becoming a single mom by choice. And the way I used to judge others’ reproductive choices now makes me cringe—I’ve come a long way.Yet I’m still frustrated with where we are as a pro-choice movement. For instance, we still don’t focus enough on the ways in which choices to reproduce are affected by financial situation, racism, transphobia and relationship status. We still seem to assume that PASS is a syndrome made up by pro-lifers. And we send around social media posts that defend abortion rights by emphasizing that abortion is integrally difficult for the woman involved, as if her suffering makes her motives pure. In short, pro-choice seems to be equal parts narrowly defined (the choice is about abortion rather than reproductive rights generally) and all over the place (PASS is not real; abortions are always hard).There’s no perfect moment in history to critique the pro-choice movement. We seem caught in an eternal battle over who gets the power of choice. And the outcomes of each battle fought are weighty: They stand to impact the mental and physical health and the life courses of roughly half the population. If you do believe an embryo or fetus is a life—and many in the United States do—then we are also hashing out whether or not everyday women, including homeless women, teenagers and others, are allowed to become custodians over life and death. Still, in light of what I’ve learned, it seems essential that we go beyond “pro-choice.” I suggest naming this new stance “pro-option.” I want us to have the option to believe that fetuses are human life as well as the option to believe that they are not human life. I want us to have the option to abort and the option not to abort—whether it’s a life or not, whether it’s a planned pregnancy or not. I want us to have the option to have babies inside or outside of wedlock, with or without a stock portfolio, at any age we choose and whatever our color or gender identity. I want us to have the option for continuing social support, however the chips may fall—whether we end up regretful or relieved, with PASS or with postpartum depression or with a “happy accident” in the carriage. Being pro-option means listening to the vast range of reproductive experiences teeming around us. Being pro-option opens up new avenues of support to women and people of all genders, whatever their background or desires or constraints. And for this reason, a pro-option movement might just grow stronger than the movements that came before it.
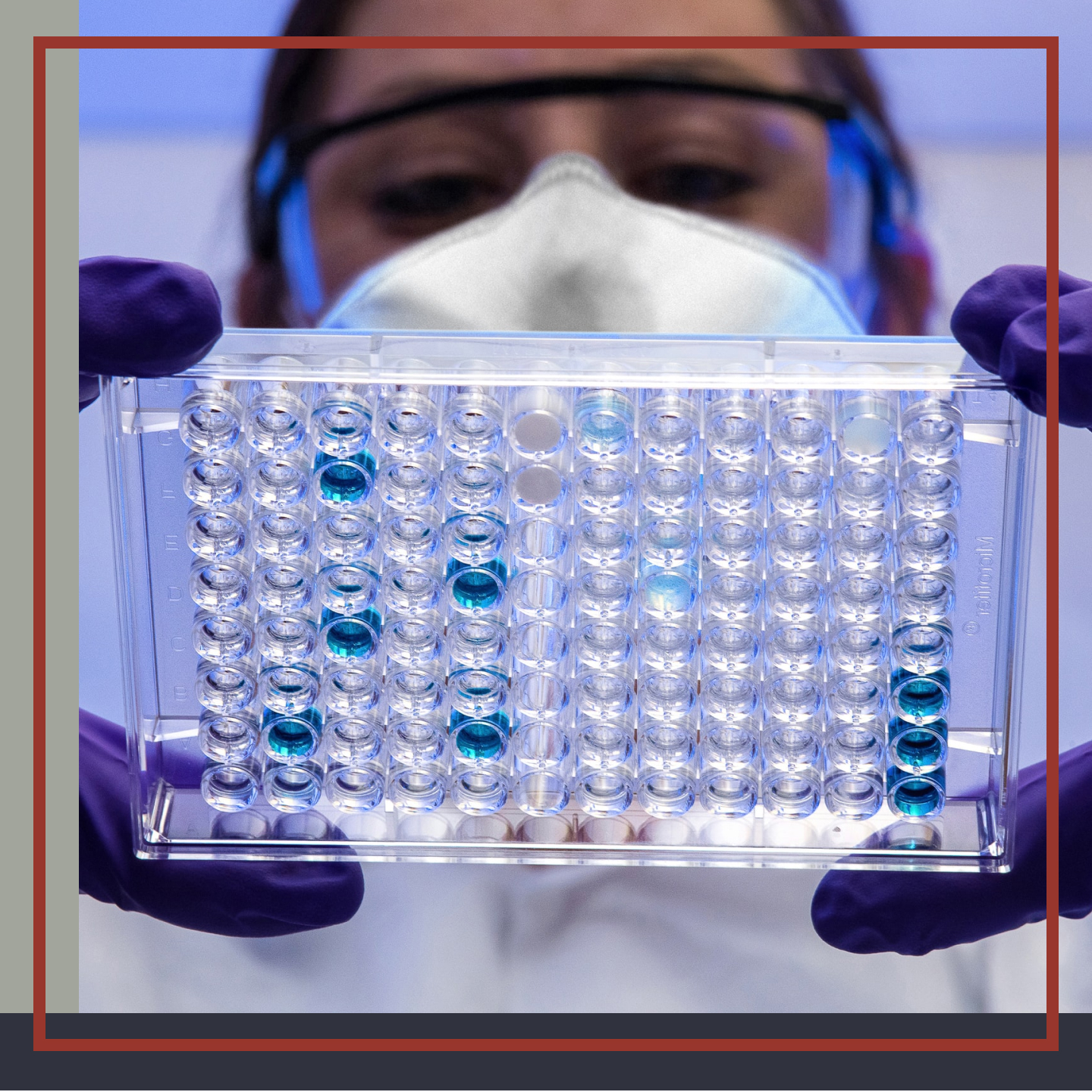
I'm an Immunologist; My Family Are Anti-Vaxxers
Dad: You’re my canary in the coal mine. This is your area of expertise. When you tell me to worry, that’s when I’ll worry.Me: Dad?Dad: Yes?Me: It’s time to worry.That telephone conversation seems like a distant memory now. It’s hard to believe it was less than 18 months ago he called. My father. Looking for advice, looking for clarity on COVID-19 from his little girl. The one with a PhD in immunology. We had no idea how much our lives were about to be upended by a global pandemic.I grew up in rural, small-town America with a tight knit extended family. Grandparents, aunts, uncles, cousins—we were all well and truly enmeshed in one another’s lives. Football games, concerts, county fairs, church services. Our holiday get-togethers were always large and chaotic. Turkey and pumpkin pie with the whipped cream piled a mile high. I loved it all. But then…I left. In my defense, I didn’t have much of a choice. Whereas my cousins chose college majors like education and agribusiness, with jobs waiting for them back in our hometown, I fell in love with immunology. And jobs in my field only existed thousands of miles away, in cities that were the polar opposite of my childhood home.Immunology is the study of how the body differentiates self versus non-self. How it mounts a defense against pathogens (i.e. bacteria, viruses) but spares healthy tissue. It’s a complex subject. More complex than an article like this could ever hope to convey. And perhaps that’s part of the problem. I have a PhD, postdoctoral fellowship and half a decade in the pharmaceutical industry and, still, aspects of the immune system confound me. Experiments yield perplexing results. The human body can be a bit of an enigma.
Maybe I should have fought a little harder for scientific truth.
When COVID Hit, I Told Family Members to Protect Themselves
Prior to the COVID-19 pandemic, my family was so proud of me. I was their big city doc, the one they looked to for answers. Does vitamin C really help with a cold? Why must I finish this antibiotic? Do we really need to be concerned about Ebola, Zika, the swine flu? On Facebook feeds and emails, I tried my best to translate the complex clinical work of myself and others to the layman. I thought I was successful at gaining understanding because my family largely followed my lead. They praised me. But in retrospect, their embrace of my advice was more likely because at the end of each communication, my “don’t worry” sign-off was exactly what they wanted to hear. Ebola, though deadly, was unlikely to see a large outbreak in the U.S. Too difficult to transmit. Zika was a worry to those pregnant or intending to conceive, but none of my family fell into that category. And swine flu? So long as we all availed ourselves of the updated flu vaccine, daily life would go on. It was a false sense of security.At the beginning of 2020, the scientific community had limited data on COVID-19. First reports from the hot zones were vague. It was a viral respiratory illness, likely caused by a coronavirus. With just this to go on, researchers like myself did what we do best: make hypotheses. Conjectures. Assuming COVID-19 behaved like other coronaviruses (i.e. SARS, MERS) then A) all that contracted the virus would have respiratory symptoms and B) the infected would spread the disease primarily after these symptoms appeared. The mortality rate, at the time, seemed comparable to the seasonal flu. Like so many others in the field, I thought humanity could handle this with travel restrictions and renewed emphasis on hygiene. If we stopped hoarding the toilet paper, we’d be OK.But as the trickle of data on COVID-19 turned into a shower and finally a monsoon, few of those initial hypotheses would hold true. COVID-19 was a far more complex and nefarious beast. There were asymptomatic superspreaders and troubling symptoms beyond the expected respiratory issues (e.g. blood clots). Plus, mortality figures for the population at large were misleading. Parsing out statistics revealed some demographics to be at a far greater risk. My demeanor, my response to family inquiries notably shifted. Lockdown, isolate. Now! It must have been jarring.

My Family Didn’t Care About My COVID Recommendations
My father handled it in stride. Perhaps because he had been my confidante at a rocky point in my own doctoral research. I had spent over two years working on the hypothesis that overexpression of one gene could cure a rare immune deficiency. It didn’t. With that failure in mind, my father didn’t seem surprised that health recommendations in a global pandemic could change. He was willing to give the researchers some leeway as they grappled to understand this novel virus. The rest of my family? Not so much. My aunt was the first to lash out. I was “letting fear consume me” in supporting the quarantine and mask mandates. The virus was still no big deal in her eyes, and unless I could “stay positive,” maybe I shouldn’t say anything at all. And I’ll admit, in their small, rural community, that first wave of COVID-19 was barely perceptible. A few elderly casualties, who arguably were soon to die anyway. The restrictions seemed overkill. Where I lived it was another matter. One Sunday, I counted and there were 25 pages of obituaries in the local paper. Twenty-five. Friends were sick; others had lost family members. I knew colleagues on the front lines, testing potential treatments, potential vaccines. And I knew the insane hours they pulled. I suppose that’s what made my cousin’s Facebook post hit so hard.Cousin Mike, let’s call him, extolled the virtues of hydroxychloroquine. He called it the “hidden cure” that we scientists were keeping from the world. I tried to reason with him. The paper that he cited had fundamental flaws. The patient number was low, the methods of blinding the study questionable. A researcher saw what he was desperate to see: hope. I looked up the clinical trials that followed that initial publication. There were hundreds registered. But no one was able to replicate the results. It wasn’t real. But Mike didn’t care. He saw no harm in taking the drug, so long as he “believed it would work.” I was stunned. I was saddened. And I was worried for the patients with malaria and lupus I knew legitimately needed that medication.In the wake of a subsequent wave of insults from Mike, I’m ashamed to say I started to censor myself on social media. I didn’t unfriend my family, per se; I just…stopped engaging.What I did post had security settings carefully calibrated to avoid their eyes. It was for my own mental well-being. But maybe it was the wrong move. Maybe I should have fought a little harder for scientific truth.
My Parents Got Vaccinated, but Other Family Members Refused
The holidays were surreal. Unable to fly home, my parents joined me over Zoom for meals made in our two separate locales while at the same time, aunts, uncles and cousins elected to covertly assemble in person, breaking official gathering size limits in the name of “tradition.” I held my breath for 14 days afterward, praying they would stay healthy. They did.And I was buoyed by the news that an emergency use authorization for a COVID-19 vaccine could be on the horizon. Historically, my family had always been receptive to vaccines. Collectively, they were even known to mock anti-vaxxers. Surely this would be what would end our divide. It didn’t.My parents were early in line to get the jab. I cried. Big heaving sobs of relief. But much of the rest of my family resisted. Their social media feeds were peppered with memes mocking the shot. And I, oddly, could see their perspective. Their only personal connection to the the pharmaceutical industry was me. And in the long time I had labored at the lab bench, I didn’t have a single drug approval to my name. Projects I worked on were still mired in safety and efficacy studies. Thus, my family’s suspicion as to the speed of the vaccine’s approval was understandable. And in their eyes, in a city far away, I did live an “extravagant” lifestyle. Prior to the pandemic, my Facebook feed had been filled with pictures from concerts, sporting events, art gallery openings. Things they considered “bucket list,” I did every week. Thus, claims of drug profiteering in their eyes would appear to have merit. And I had lost my means to defend myself, to defend science. No questioning emails came my way.
The situation remains tense.
I Feel Like My Life’s Work Is Being Gaslit, and It Will Only Get Worse
I wish there were a better ending to this article. The situation remains tense. And I feel for my parents. They’ve placed their faith in me, in science, and sacrificed precious time with loved ones as a result. As the Delta variant surges and the hospital in my hometown reaches capacity, I just hope and pray we all continue to skirt disaster. Because I love my family. Through it all, I love them.My story is not unique. Many friends and colleagues in science find themselves in a similar position. We’re tired, so tired. Caught in some twisted cultural gaslighting of our life’s devotion. What comes next? My greatest fear is that other therapies being developed for cancer, autoimmunity and heart disease may meet a similar fate to the COVID-19 vaccine. Rejection, no matter how effective. How do we bridge this divide?

Medical Apartheid: Disabled People Deserve Equality Too
In the 30 years since the Americans with Disabilities Act was passed, being disabled in America is not accessible. This stems from what I like to refer to as “medical apartheid.”Accessibility starts with basic human rights. Housing is a human right. Health care is a human right. Safety is a human right. They are very basic needs, and the ADA guarantees none of them. Factually, the ADA ensnares disabled folks into forced poverty, further marginalization in society, state sanctioned violence, lack of health care and lack of representation. And in true American fashion, it condones racism, sexism, homophobia and ableism.One might ask, “Doesn’t the ADA specifically protect disabled folks? If not, why does the ADA even exist?” That would be a great question, one that I myself am forced to reckon with daily. Though, when I say I’m forced to reckon with that reality, it pales in comparison to the rest of the disabled community.
Last time I checked, we were still human beings.
I’m an Advocate for the Disabled Community
Let me start off by stating that I’m a white, cis male. I am 6-foot-3, and I’m not visibly disabled. I have been permanently disabled (yes, that's a legal designation) for eight years, diagnosed with bipolar I and post-traumatic stress disorder. Even with a permanent disability, the amount of privilege that it affords me stands in direct contrast to most disabled folks who are not white, cis men. Despite this, I have a much harder time taking care of myself and leaving the four walls of my home than I would like to admit.I’m lucky to have a home. I shouldn’t be able to afford one, especially with the $1,035 given to me monthly by SSI/SSDI. While it's amazing to be able to have a place to live, the ADA legally guarantees me public housing thanks to Section 8 and/or HUD. But my building is inaccessible for wheelchair access; this is problematic, to say the least, for the disabled community. While I’m eligible for assistance, I am on never-ending waitlists to receive assistance with rent payments and access to transportation, all while forcibly living below the poverty line. Millions die on the streets waiting for a decision from the SSA to receive funds, and the lack of wheelchair accessibility is at a rate of less than one percent of homes in the United States. To help combat this, I do advocacy work for 99 percent of my waking life, most specifically centered around racial justice, the erasure of patriarchy, LGBTQ+ justice, animal rights, the erasure of prisons and disability justice. So yes, I’m an intersectional abolitionist. I only mention this to give context to who I am and how serious these issues are. I would be remiss if I said that any one person can advocate for the entire disabled community effectively. Nobody can do that alone. There are far too many needs for accessibility—with differing disabilities, locations and lack of awareness on a national level—for any one person to be able to advocate for the entire community. This is due to a general failure of local, state and federal governments to implement almost every aspect of the ADA. Schools, workplaces and doctor’s offices are happy to ignore its existence as well.In Los Angeles County, there were zero ADA-accessible vaccination sites. The assumption that folks with disabilities have access to a car or support from somebody who can drive them to a vaccination site in the most populated county in the United States should be extremely telling in regards to how often the ADA is violated with impunity on a governmental and health care level. It ended up taking me days of phone calls to rectify this issue with city officials. The city, the county and their health departments relied on nobody saying anything. Sadly, institutions consistently violate the rights of disabled people with the assumption that nobody knows their rights. I can say with certainty that the city wouldn’t have felt obligated to address this issue without the privilege I hold, even though I’m disabled.

Disabled People Face Discrimination in a Variety of Ways
I’m now going to address medical apartheid, best described as the accumulation of school-to-prison pipelines, overt racism in health care, forced poverty/housing and state-sanctioned violence. More than 50 percent of people killed by police in the United States are disabled. Adding insult to injury (quite literally), over 40 percent of the houseless population is disabled. We live in poverty at well over the rate of people without disabilities. Poverty makes access to health care, education and resources much more difficult, while also making disabled people and their children much more likely to be maimed by police, chained by police and killed by police.Student with disabilities are twice as likely to face punitive measures in schools as those without disabilities, and non-white disabled students can be punished harsher and longer than white peers for similar offenses. Law enforcement’s presence in schools, many of which have police and no counselors, very clearly turn these punitive measures from schools into criminal cases. We’re talking about kids!The majority of these children have household members already suffering from this oppression, further destabilizing families, which in turn, destroys entire communities. If these children need care and diagnosis of that trauma, they likely won't receive it anywhere outside of a cage. To this point, it’s worth noting that the U.S. prison system is the nation’s largest mental health care provider. This is morally incomprehensible, yet nobody cares. If they did, legislation would be written and passed.

Give us liberty—you’re already giving us death.
Our ADA Rights Are Rarely Being Enforced and Practiced
It's appalling that society puts the labor of disability advocacy onto the disabled community itself. If you just scoffed at that comment, when was the last time you looked into disability issues?The ADA was always discriminatory in nature, and that is an entirely different conversation regarding gender binaries, sexual orientation and other “choices.” This has gotten better with each revision, but the rhetoric spoken during these committee meetings by our elected officials on public record is inflammatory, hateful and ableist in nature. This issue is largely due to the lack of representation in government, companies and institutions in the disabled community. We don’t have representation. More than 25 percent of the United States population is disabled, and we aren’t as small in number as most people would presume. Almost none of the ADA rights guaranteed to us are enacted, and there isn’t any realistic oversight on this, let alone accountability or solutions. SSA also implements nefarious policies around work—if I earn more than $2,000 a month, I lose my health care. If I have more than $2,000 in my bank account at a time, I lose my health care. Tragically, the ADA allows employers to pay disabled folks less than minimum wage. I can personally attest that they love this rule. I’m never paid what my non-disabled peers are for the same labor, oftentimes skilled labor. Last time I checked, we were still human beings. It is very important to point out who is responsible for this. We need to do more. Everyone perpetrates this, not just the U.S. government. In all of the work I do with nonprofits, which specifically state things like, “Disability justice is intersectional to liberation,” I’m met with heavy resistance when I address disability. Nobody wants to talk about it. Let’s talk about it please. These ripple effects destroy families and communities, while oppressing the most vulnerable population of an already vulnerable population. Stop hoping we all die when you aren’t busy actively killing us. This isn’t 1930s Germany, but it feels like it when you’re disabled. The ableist speech is killing us. The forced poverty is killing us. Give us liberty—you’re already giving us death.

Liberal Healthcare Policies Fail the System Every Time
This year, the State of Washington passed a progressive healthcare policy that aims to address services for low-income families and issues with the state’s Medicaid budget. The new Long-Term Care Trust Act tackles the idea that as we age, poverty and financial distress will prevent Washington residents from being able to afford long-term health services such as nursing care. Washingtonians for a Responsible Future states that: “Median retirement savings for people over 65 is just $148,000, while the lifetime cost of care averages $260,000. Medicare covers only limited long-term care for skilled nursing care or rehabilitation, leaving most people uninsured for their long-term care needs.” The fix for Washington residents? A tax that forces you to pay into your own nursing care funds.What’s interesting about the long-term care tax isn’t that Washington’s Governor Jay Inslee has no faith in his residents to control their own spending but that each resident’s return when they need access to care is laughable. Here’s the big win for your lifetime contribution to your own spending account: a maximum benefit of $36,500. If that doesn’t sound like it will do much for you when you need living assistance, you’re right. According to the Genworth Cost of Care Survey in 2020, a nursing home in Seattle will cost you around $10,621 per month. The tax itself currently stands at 58 cents for every hundred dollars in income, which may not sound like a large sum of money upfront. However, the median income in Seattle has surpassed six figures, meaning young, healthy residents working average Seattle salary jobs are holding up the policy for the rest of the state. If you’re reading this from outside of Washington and chuckling to yourself, trust me, I get it. But if you’re living in the Seattle area, you understand that making $100,000 per year means you’re struggling; the cost of living here is laughable and frankly, insulting. If Amazon, Google or Boeing ever leave our state, we will crumble—rightfully so. What if you end up not needing assistance at all? Perhaps you stay healthy until the end of your life or pass away without prior disability. You, or your family, will never see your savings returned. What’s even worse, if you choose to relocate out of the state at any time, your funds won’t be following you along. None of this matters to Washington lawmakers, who are more concerned about trying to fix our failing Medicaid program and skyrocketing health insurance costs by increasing our taxes. Why continue to fund inadequate leaders?
If that doesn’t sound like it will do much for you when you need living assistance, you’re right.
I Tried Opting Out of the Tax—but Was Denied a Private Plan
If you’re like me, the thought of paying into savings you may never utilize or get a return on feels like a financial gamble. What’s the harm in saving my own money? Even if I put in less than the $36,500 over my lifetime in tax, most individuals place their retirement funds into stock for higher growth regardless. At the very least, I always have access to my savings if I need it in an emergency. The point of the tax isn’t to be charitable to other residents at face value, though you staying healthy or passing away early certainly benefits others when your funds are then shared. As a contributing member of my local community, I spend more than 58 cents on the hundred dollars to charity and believe I can handle my own finances in the way I see fit. The only silver lining to the new policy is the “opt-out” option.Opting out isn’t really opting out, though. By law, any resident who wants to avoid the tax must either have or obtain their own private long-term care policy to prevent being a “burden” to the state. Regardless of Washington’s extremely high taxes and healthcare costs already (a single-person plan can cost up to $600 per month with poor drug coverage), the local government still can’t seem to get the cost of living right for West Coast dwellers. Because I don’t plan on staying in Washington for more than another decade, I decided to search for my own private long-term care policy in addition to my current health insurance plan.I was one of the early residents jumping on the opt-out option, immediately choosing between two plans that best fit my budget and most closely resembled the amount I would be paying into the tax based on my income. The process took months, with multiple meetings with my advisor and pages of paperwork to fill out. When my application was finally in, I waited for a phone interview to discuss my health history. As a licensed healthcare provider myself, I wasn’t too worried about my interview and knew the questions I would likely be asked: when my last tobacco encounter was, how much I weighed or my family history of cancer. While I was waiting for my interview, my advisor began to express her concerns with insurance companies doubling and even quadrupling their premiums. With countless panicking residents feeling backed into a corner, many began to opt-in and then drop their plans to escape the tax. Because Governor Inslee only gave Washington residents a few months’ notice prior to the tax, insurance policy underwriting was backing up and ultimately led to many pulling out of offering plans altogether. Now private policies were for the lucky and the wealthy because private organizations will never keep up with impossible financial government demands. I felt cheated. My phone interview finally came, which lasted about an hour. I wasn’t just asked the basics; I was asked questions about my future choices that would pose any potential danger to my life. Questions like, “Do you plan to climb a mountain? Do you ever plan to skydive? Have you ever had a blood draw in your life, and what were your results?” As I answered each question honestly, I suddenly knew which question was going to catch their attention. I have had minor lifelong epilepsy, a specific kind of seizure condition called focal onset aware seizures. Despite never losing consciousness during a seizure, only having one seizure in five years and taking my anticonvulsant religiously, I was denied a policy. Now, only two months away from the opt-out deadline, I’ve been fighting for a full medical record review and ultimately don’t know whether I will ever get private coverage. Because of something I have no control over, I’m left with no choice but to pay into a tax I will never utilize when I leave my home state.

I felt cheated.
Socialist Health Care Values Can Be Better Utilized in Capitalism
It’s funny; when I hear millennials talk about the benefits of socialist health care policy, keywords like “equal,” “fair” and “moral” often overtake the conversation. I come from a military family where both of my parents served in the Army, my father-in-law in the Marines and my grandfather in Vietnam. I was with my grandfather the day he passed from a lifelong Agent Orange lung injury and feel forever indebted to him for his sacrifice. My family all fought for American freedom, the freedom to choose our own path. Citizens of communist and socialist countries aren’t allowed this privilege. Their leaders feel they know best, but a baby born in America will grow up with unlimited potential. I cringe when I see my friends on social media post about socialism from their $1,000 iPhones, wearing nice clothes, from their favorite coffee shop. They’ll never know what it’s like to grow up in true poverty, lose a father to the draft or never have the option to handpick their medical provider. Words like “fair” or “moral” are tossed around like they have no weight behind them.In 2021, capitalists are painted as selfish or careless for simply wanting control over their finances. While I believe every individual should be as charitable as possible, and many capitalists are, forcing taxes upon residents to pay for their healthcare services under government guidelines has been unequal, unfair and immoral for me and many residents along the way. My experience with the Long-Term Care Trust Act is a perfect example of how a big-government program can easily go sideways. I’m left asking myself, “Why can’t I take my funds with me when I leave? Why can’t I get coverage just because I have a chronic condition? Why can’t my funds be passed down to my family if I die without disability?” When a socialist-type health care policy hits your state, you should ask yourself the same questions. You should also ask yourself why a policy was passed without your vote. We trust our politicians to keep our best interests in mind, but they often make policies without a public opinion.The values behind socialism are merciful, compassionate and kindhearted. Those values match the values of the everyday American capitalist as well. Our healthcare system isn’t perfect, especially in Washington state. But control of my finances allows me to contribute to my health in the best way I see fit without stripping me of financial investment. This way, I can share my additional wealth, whether with finances or in volunteer time, in community-building ways. If you’re a socialist, you can carry your values into society without supporting unfair health care policies. Serve at a low-income mobile health clinic, donate your daily latte money to a hospital or nursing home charity or start a fundraising campaign for an individual in your community that you know needs assistance. As Winston Churchill once said, “The inherent vice of capitalism is the unequal sharing of blessings. The inherent virtue of socialism is the equal sharing of miseries.”

My Horrific Experience With Anesthesia
After having several procedures in my life, including an emergency C-section, emergency dilation and curettage (D&C) and others that required sedation, the surgery I was scheduled for just a few weeks ago seemed like a walk in the park. My surgeon explained I would only be under for 60–90 minutes max and that as long as there were no “surprises” while in the operating theater, I would be allowed to recover and go home by lunchtime. That was the plan. But that’s not at all what happened.I’ve had my fair share of medical surprises that sidelined me. There was the time I needed several bags of blood due to a hemorrhage doctors couldn’t get under control. Or the time I went to the OB-GYN for an ultrasound at 36 weeks pregnant but was sent across the street to the women’s center due to placenta previa concerns and held my child in my arms less than two hours later. I know to expect the unexpected and roll with the punches.
This was not normal.
I Was Looking Forward to a Quick Procedure
This day, however, was much different. After three nurses failed to get an IV into any vein in my body during pre-op, the anesthesiologist appeared, ready to apply his expertise. Super witty with a bubbly personality, he seemed to really love his job. He explained that he enjoyed being the one person that had the power to relieve people from their pain and give them a bit of a rest while the surgeons did their thing in the operating room.That made sense to me because each time I was put under, I looked forward to it. This was a rare moment when I wasn’t in pain or fretting over the issues I was dealing with in waking life that severely altered my quality of life. That swift descent into sleep is something that I welcomed. And of course, waking up from anesthesia, having completely left my filter behind and saying ridiculous things, had always been the highlight in the middle of uncertainty, anxiety and fear. So going into this procedure, I was excited to take my two-second nap. When you go under, you’re extremely sleepy for a few seconds, then you wake up in a different room having already had the procedure done. It’s a really strange feeling, but it’s also refreshing to know you’re on the other side of the surgery itself and on your way to recovery.The anesthesiologist found a tiny vein on the inside of my left wrist, inserted the IV and taped it down. It was so close to the skin that if I bent my wrist at all, you could see it try to break through the skin. It was painful. They began to wheel me back to the operating theater, and I started to feel weightless from the first burst of whatever was pumping through my IV. Lights began to blur, and the sounds around me were muffled. The anesthesia was starting to kick in. Let’s get this over with.

I Woke Up From Anesthesia in Excruciating Pain
By the time I made it to the operating theater, I watched nurses and surgeons walking around all masked up, but I didn’t see anyone I’d been introduced to just a few minutes earlier when they were getting me prepped. Masked figures walked around above me, sticking patches all over my chest and my hips. The one person I did recognize, a beautiful, blond, pregnant nurse that had said she would be by my side through recovery, was above my head putting a gas mask on my face and asking me to breathe in slowly. I remember breathing in once, twice and on the third breath, falling under.I woke up at what felt like one second later in the most excruciating pain I’ve ever had in my life. I felt everything. Every sensation. The cuts, the stitching, the pressure from having just had the procedure done and organs clearly tugged and pulled in different directions. A burning hot knife felt as if it was being slowly pushed inside my stomach. I remember screaming and frantically begging for help. I was connected to machines via tubes on both sides of my body. I remember looking around the room and the nurses all looking at me like I had eight heads. They were in as much shock as I was and began to shuffle all around me—checking vitals, looking at my IV, an older nurse tap, tap, tapping at the computer. I remember holding my abdomen where I had just been sliced open and saying, “It hurts, it hurts! Please, God, help me!” I didn’t recognize anyone nearby, not even the beautiful mother-to-be, as promised.Soon after, I woke up in a different room. I wasn’t sure how I got there or how long it had been since my first time waking up, but it felt like I’d just blinked my eyes again. I was alone. The pain was still there, and it was every bit as intense as before. I started back up with the “please help me, it hurts” bit because it did, very badly. This was not normal. The windows were open and the sun was blinding. There was a TV, bathroom, etc. I had compression cuffs on my legs and wires and tubing connected to me still, so what was going on? What happened? Was I OK? Had I gone into shock? I was still screaming in pain when my husband walked in. I wasn’t aware of his arrival until he touched my arm to try to calm me. I looked up at the clock. It was 2:15 p.m. My surgery started at 7:30 a.m. Why was I in this room alone, and what happened to all of that time? Did something go wrong during the surgery?
I felt everything. Every sensation.
My Surgery Experience Was Beyond Traumatic
A new nurse walked in, telling me they had ordered something for my pain and she was going to get it. When she returned, I tried to ask her what happened, but she said she was just assigned to me as a patient and hadn’t been part of the surgical team. The nurse gave me two tiny pills, which I took, my throat still scratchy and sore from the tube that had just been removed. The medicine kicked in some time later, but as with any anesthesia, my sense of time was nonexistent. A young male doctor I hadn’t been introduced to then came in and explained to me that the surgery itself was perfect, textbook even. Everything went well, and there were no complications. Blood was not needed, and the surgery was completed in just under 90 minutes. The doctor explained to me that I had woken up early, before they were ready for me, and they weren’t sure why. Though the surgery was technically complete, no pain medicine had been administered at that point. They had just transferred me from the operating room when I woke up prematurely, surprising the staff in the recovery room and freaking out all the patients around me who heard my screams. He said they wanted to keep me overnight to observe me but explained that as long as I could pass a few tests, I could go home if I wanted. So I pushed through the pain and started the tests, proving I was able to walk, and they agreed to discharge me. I was released a few hours later, not making it home until 5 p.m.I had still not seen my surgeon since before going under and was eager to get her account of what happened. The next day, the beautiful, blond, pregnant nurse—who was not in recovery, as promised—called to check on me. She corroborated the male doctor’s account of events, neither of them having an explanation as to why I woke up before I should have. I go in for my six-week post-op appointment next week and hope to get answers as to exactly what happened and to account for the hours of lost time. What I can say is this experience was beyond traumatic and something I don’t want to live through more than once. I’m one of those rare individuals that knows what surgery feels like without pain management. It’s a badge of distinction I wish I’d never earned.

The American Healthcare System Has Disrupted My Physical Therapy Practice
I’m a physical therapist, and my occupation has many different meanings to many different people. To some, I’m a personal trainer; to others, I’m a massage therapist. And to those that understand my holistic approach to therapy, they see me as a healer. Over the years, I’ve experienced a wide range of patients with different expectations of me.Through the lens of those I treat in the clinic, I’m very helpful and am able to guide them through their recovery process from an accident, injury or recent surgery. Those that have had the experience of my home treatments understand the way my hands can heal them and that the use of energy work tied together with manual therapy can manipulate their bodies to have incredible results.Time in the health care world is everything. Let me explain what I mean by that. Time, for a patient, revolves around several factors: recovery time, initial evaluation time, between-treatment time, during-treatment time. For a therapist in an office, time revolves around only two factors: reimbursement and commute. Time is also a valuable tool when you’re appropriately being compensated, and you can spend it by helping to heal a patient and reduce the number of sessions and length of their recovery with focused therapy and treatment programs.I’ve been working in my field for a short time in comparison to most physical therapists, but I’ve been able to treat many different kinds of patients and clients from all walks of life. They range between homeless patients that don’t have any insurance to the extremely wealthy clients that prefer not to deal with any insurance companies because they’d rather have no record of treatment.
Before she could get her shoulder all the way up, her sessions ran out and it took her several months to get another referral to continue her care.
Clients With Different Health Plans Can Cause Major Complications
As an employee of several different therapy groups, I had been instructed to quickly discharge patients with low-paying health maintenance organizations (HMO) and encourage them to use a home exercise program (HEP), while keeping on patients with higher-paying preferred provider organization (PPO) plans. The reason for this is because the reimbursement rate for PPOs is significantly higher than that of HMOs.The job becomes more difficult when HMO clients are scheduled with other patients; they get stacked during the same time slot without being staggered during the actual appointment blocks. There is a huge imbalance in this country's health care system, and it is only going to get worse as long as insurance companies are setting rates based only on volume and not outcomes. Bringing therapy to the masses is a very difficult task because properly educating patients and helping them through their recovery journey takes time. When time is taken away, you’re left with half-treated patients that aren’t able to be independent with a HEP, or with patients that require more sessions when they’re discharged from care. One time, I was treating a patient diagnosed with a frozen shoulder. She was finally starting to achieve some of her functional goals—like raising her arm overhead to get objects off of high shelves—but before she could get her shoulder all the way up, her sessions ran out and it took her several months to get another referral to continue her care. The intent of this article is not to belittle HMOs as a health insurance strategy—they work very well for people that are healthy and don’t require a great deal of care. They also work well for those able to advocate for themselves in the system. I’ve seen a lot of people get coverage for different resources that I didn't think were possible, but through the proper advocacy, they got what they needed.

There is a huge imbalance in this country's health care system.
It’s Important You Understand the Medical System and Ask the Right Questions
One of the major problems that I’ve seen working within the HMO system, however, is the need for referrals to get services. That means that the primary care physician (PCP) is the gatekeeper of care. Without a recommendation from your PCP, you’re not eligible for further resources. An example of this is if a patient has some kind of medical issue that the PCP does not know how to, or is not willing to, handle on their own. The physician then creates a referral to move the patient to a specialist. The specialist could refer the patient to get imaging, and then to a surgeon, physical therapist or someone else. This is a big issue because it can take a lot of time for referrals to be approved by the HMO. I’ve seen this play out in very catastrophic ways—with a patient starting with a small pain in their shoulder then needing to wait months to see the orthopedist, then a few more months to get imaging, followed by more waiting and then finally getting referred to see the physical therapist. By then, they’re unable to move their arm above their head without extreme pain. The medical world is complex and continues to get increasingly complex as time goes on. Through my short but thorough years of experience, I have learned that knowledge is power when it comes to knowing and understanding our medical system. And if you really need something done, call offices and check back with doctors to make sure they’ve filled out the paperwork to stay on top of your health. Keep asking questions.

Long Live the Midwife: A Corporatized Hospital Birth Deepened My Medical Distrust
My first four children were delivered by midwives in two different countries, and everything went fine and dandy (something especially easy for a dad to say). But when our fifth child was entering the world, my wife and I both got a rude awakening that we hope to never endure again. Expecting parents: Beware. Being born is big business! Thanks to a possible complication with the delivery, my wife and I were involuntarily thrust into the world of corporatized, hyper-medicalized baby delivery. It’s an industry like no other. Cross Big Pharma with Big Brother and you get a sense of it. To call our experience unpleasant and dehumanizing would not do it justice. The arrogance of the doctors and their fiendish desire to inject all sorts of dubious foreign substances into our new baby was beyond outrageous. Before our precious new child even arrived, the staff brought in a tray full of syringes, droppers and more. More on that later.
Delivering a Baby Right With a Midwife Birth
First, it helps to know what delivering a baby can be like when done right. Our first two children were born in Sweden. And while I loathe government-run health care systems, the midwives we had were kind and very accommodating to whatever my wife and I wanted. When it was time for the baby to arrive, we did go to the hospital. At first, it seemed weird to have no doctor. My family in America was shocked. But as time went on, it became clear that the midwives knew what they were doing and that our wishes as parents would be respected. When we declined the vitamin K injection, that was it. No high-pressure sales tactics. No guilt trips. No shaming. No treating parents like idiots or worse. Just moving on to the next question about what we wanted in order to offer the best experience possible. The Swedes don’t even vaccinate newborns. And when the time came, all we had to say was “No thanks.” The irony surrounding the respect for “consumer choice” displayed by a government-run healthcare regime in a nation known for hostility to individual liberty and parental rights did not hit me until our horrific experience at the American hospital. Later, I discovered that Swedish midwives are sometimes forced to participate in abortions. That shocked me to my core. How could the same woman who just helped deliver my baby also be involved in slaughtering unborn babies in their mothers’ wombs? Sick! Fortunately, I didn’t learn that until after we left Sweden, or I might have freaked out knowing that the hands delivering my precious children also participated in shedding innocent children’s blood—children who probably would have sounded and smiled just like mine.

Birthing With a Midwife vs. a Doctor at an American Hospital Could Not Have Been More Different
My next two children were delivered by a hippie midwife in America. Again, aside from the pain inherent in childbirth, it went as well as it could. The midwife and her assistant were kind and respectful. We were never pressured to accept anything. Just like in Sweden, when we declined, that was the end of it. When it was time for our fifth child to arrive, we did what we had always done: We called the midwife, called our friends to take our other children and hopped into the car to head to the midwife. Because my wife worried about not being able to go back into our home if anything traumatic happened, we never did a home birth, opting instead for the midwife’s facilities.When we arrived, it was awesome. The delivery room felt like a beautiful bedroom. There was a king-size bed, jacuzzi, couch, paintings on the wall, a splendid bathroom and more. It was better than any hotel I’ve stayed in. The midwife on duty checked on my wife from time to time as she kept track of progress. Finally, it came time to push. The screaming began and got louder, just as it always has. My wife is very modest, so she asked the midwife not to feel around too much down there. But as the screaming got louder and more intense, and a weird pain in her leg got worse, and the baby refused to come, the midwife finally decided to see what was going on. Well, she determined that something—I won’t get too graphic—was swollen for some reason. So, she gave us a choice: Try at the birthing center, knowing it may be painful and complicated, or call an ambulance. Within ten minutes, paramedics showed up, looking terrified that this screaming woman might give birth in their ambulance.At the hospital, an OB-GYN came into the room and examined my wife. Tons of nurses and other people—not sure exactly what they were for—came in too. And then I saw it: One of the nurses or orderlies wheeled in a tray filled with syringes, vials and stuff I didn’t recognize. As I held my wife’s hand, I made a mental note.The first thing they demanded was a COVID-19 test on my wife. She was screaming in pain, so I told them we would decline that and that we did not have COVID. “Well, if you don’t let us test her, we’re going to have to treat you like you have COVID,” the nurse said. “We may have to separate you from the baby when it arrives.”Are you freaking kidding me? I thought. What kind of insane asylum have we landed in? After talking briefly with my wife, we decided to consent but only under duress. It went downhill from there.
It went downhill from there.
The Medical Staff Treated Me Like an Uninformed, Irresponsible Parent
Literally five minutes after we got in the room, the baby arrived. Everything went smoothly, though I overheard the staff talking smack about our decision to use a midwife. Then the pediatrician came into the room to inspect the baby. Almost right away, I saw her going for the tray. And so, without hesitation, I told her we would be declining all vaccines, as well as the vitamin K shot and antibiotic ointment for the baby’s eyes. “Sir, I really must insist,” the pediatrician told me. My blood was boiling, but I tried to keep calm. “Doctor, I must insist also,” I responded, knowing my rights under state law and my responsibility as a parent. “As his parents, we do not and will not consent to any injection or vaccination of this child.”“Well, I’m going to have to go get you some literature,” the doctor snarled before storming out of the room.At that point, we were informed by a nurse that they were going to keep us for “observation” for “another couple of days.” Officially, it was because my wife had taken some test five weeks ago that supposedly had to have been done four weeks prior to delivery. The baby was late, after all. But in my mind, it was retaliation.

What Happened Next Only Deepened My Medical Mistrust at the Hospital
Between an endless stream of “checks” with people barging into our room, the pediatrician came back with a bunch of propaganda from the Centers for Disease Control and Prevention (CDC). It’s hard to think of a source I would trust less—they’ve been doing the bidding of Big Pharma for decades. With all their insanity surrounding COVID, I would not trust the CDC to clean toilets. My wife and I happen to be extremely well-informed on this issue. By divine providence, an editor asked me to look into the swine flu hysteria over a decade ago, right before our first child, for a cover story. Thank God. At that time, I had no reason to be skeptical of vaccines. But the more I learned, the more I realized something was amiss. It started when I looked at the federal government’s 1976 swine flu vaccine program that left large numbers injured and paralyzed. According to many sources, the shots did more damage than the flu itself.Then I dug deeper. I found congressional testimony by polio vaccine creator Jonas Salk sounding the alarm about polio shots. Reading study after study, it became clear that vaccines were not nearly as “safe” or “effective” as Americans had been led to believe. Finally, I bought some books on the subject. It was settled: We would not be vaccinating our children. To this day, I feel it’s among the best decisions we have made, and we have made a lot of great ones, like homeschooling, for example. We know families whose eldest child was injured by a vaccine, while the unvaccinated younger ones are totally healthy. At the American hospital, the pressure was on. But not one piece of the propaganda the doctor brought me included a single word on the risks—and there are many risks. Just read the package insert, or look at the billions the U.S. government has paid out to victims of vaccines ever since Congress granted vaccine manufacturers total immunity from liability.When I asked the doctor for the package insert, she got really mad. “You’ll have to go down to the pharmacy if you want to see that,” she fumed. Hmm. Why all the obfuscation? Why not bring honest, accurate information so parents can offer informed consent? This was beyond disgusting.The vaccine they were peddling was for hepatitis B, typically transmitted through sexual activity or intravenous drug use. Confident that my baby would not be engaged in either for a long time, I informed the doctor that we were standing by our decision and would not budge. As for vitamin K, which is supposed to prevent internal bleeding in the very rare cases in which it happens, after carefully weighing the risks and benefits, we declined again. Yes, there is a risk, but there are risks to everything. One study I found linked vitamin K shots with almost double the risk of leukemia. Plus, I trust God more than the corrupt medical establishment.
With all their insanity surrounding COVID, I would not trust the CDC to clean toilets.
I Know the Science Behind Anti-Vaccination, and I Won’t Be Coerced Into Giving My Baby Vaccine Injections
To be clear, I have no doubt the doctors involved really believed we were just idiots who had fallen for “anti-vax” propaganda on the Internet. And I have no doubt that they were trained to think just that. They thought they were doing the right thing. But what they did not realize is that over the last ten years, I’ve spoken with and interviewed dozens of prominent doctors on this subject. In fact, I had almost certainly learned more about these medical interventions than they had in medical school. Don’t believe me? Ask a doctor how much training they’ve had on the science of vaccines. You will be shocked.After a couple of days of this back and forth, I was starting to get concerned that they would either keep us longer, or worse, call Child Protective Services. While confident we would beat them in court, the ordeal would be a costly nightmare. Naturally, I didn’t let them out of my sight with our baby. Concern bordered on fear. Finally, after three long days of anxiously waiting for permission to leave, I insisted we had to get back to our other children. They reluctantly processed the paperwork and let us out. Phew! It is beyond sad that doctors and hospitals treat well-informed paying customers—and parents who love their child more than anybody else on the planet—like idiots or worse. It’s an outrage. After COVID, polls show declining trust in the medical establishment among Americans. Frankly, I’m surprised it’s even that high. Long live midwives.

How I Dealt With a Teenage Epilepsy Diagnosis
On October 11, 2014, I had my first seizure. Like every Sunday, I was on the way to my dance class, which required a drive to the train station. At 14 years old, my whole life would soon change, and I didn’t even know it yet. While waiting for my train to arrive, I suddenly fell into my first ever tonic-clonic seizure and hit my head on a metal pole. The seizure lasted for about two minutes, and when I opened my eyes, I didn’t have a clue what had just happened. I was lying on the floor, looking up at strangers. The paramedic asked me if I was OK, but I couldn’t respond. I don’t remember much from that day; however, my mom told me it took about 20 minutes for me to come around. Before I knew it, I was being lifted into an ambulance. I was tired and scared and didn’t know what had just happened to me. The hospital staff kept me overnight because of my severe head bump and because I had just experienced my first seizure.If you had asked me what epilepsy was when I was 14 or younger, I would have told you it was some sort of illness that makes people have seizures when they look at flashing lights. Little did I know that there is so much more to it. I wish more people knew this. Epilepsy is a hidden disability where sudden bursts of electrical activity in the brain cause different types of seizures. There are about a dozen types of epilepsy, which play a role in the type of seizure you have. The symptoms can involve uncontrollable jerking, collapsing, stiffening and other strange sensations in the body. Side effects often come more from epilepsy medication; however, there are a lot of restrictions that can come from being diagnosed with this disability. The main treatment is often medication, but there are other kinds of treatment such as brain surgery, the vagus nerve implant and going on the ketogenic diet. It is not proven that epilepsy can be cured; sometimes it runs in the family or it can be caused by a severe head injury.
I had no idea how much the side effects from the medication would affect my mental health.
I Was Diagnosed With Generalized Epilepsy
The next day, the doctor told me not to worry, that it was probably just a one-off seizure and to just keep an eye on it. But four days later, I experienced my first absence seizure, which is when you blank out and can stare into space for up to a few seconds or even a couple of days. This scared my mom a lot because even though my eyes were open, I wasn’t responding to her. After this, we knew something was wrong, but the doctors just kept telling me that it was my menstrual cycle or that I was just stressed out. It wasn’t until October 2015 that I got diagnosed with generalized epilepsy. I didn’t really know much about it—my mom dealt with all the hospital and doctor’s appointments, and I just had seizures. Then I got put on my first medication, and I just remember thinking, “Thank God it's all going to be over.” Little did I know it would get ten times worse. I had no idea how much the side effects from the medication would affect my mental health—I experienced memory loss, blurred vision, difficulty processing information, and on top of all this, I had to deal with the life of a 16-year-old in high school.I was feeling sorry for myself, and I blamed a lot of my problems on epilepsy. I would get upset and angry over the smallest of things and then have a seizure and have to go home. I missed a lot of school due to seizures, and I gave up quite easily. I didn’t push myself through the tough time I was having; hence the reason I failed most of my GCSEs.
I hit rock bottom, and I didn’t know what else to do.
I’ve Become an Advocate for Those Impacted by Seizures and Poor Mental Health
Going to dance college with no GCSE worried me. Some days, instead of going to school, I would get the bus into town to try and find a hospital that could help me. Nobody would listen. Hospitals told me to go home, and treatment centers told me I needed money. I felt lonely. I wanted to give up, so I took the easy route and decided that I didn’t want to carry on dancing. Quitting college was very out of the blue, and I had no idea what I was going to do. All I knew is that I wanted to be happy. I thought a few weeks off would be fine, then I’d get myself a job to earn some money and everything would be OK. I was very wrong. I got bored of doing nothing every day, and every employer kept turning me down. It was almost like no one wanted an epileptic girl working for them. I hit rock bottom, and I didn’t know what else to do.Eventually, I started receiving counseling for my mental health, and my mom pushed for more doctor’s appointments. That led me to opt for vagus nerve stimulator surgery, which allows me to now feel when a seizure is coming on. My mom also got me to volunteer at a local dance school, which gave me something to do instead of feeling sorry for myself. I really enjoyed teaching little kids to dance, and my mom has now suggested I start an apprenticeship in child care. I wouldn’t be where I am today if it were not for my friends and family. I am now a level 2 early years practitioner, and even though I was always so embarrassed by my epilepsy in high school, in my spare time, I spread awareness about those impacted by it. I’ve come to terms with the fact that I live with a hidden disability and I shouldn’t be embarrassed about it. During lockdown, I even started making TikToks about my crazy stories and answering people’s questions about epilepsy. My videos have gone somewhat viral, so I’ve decided to start an Instagram page. Now I’m doing whatever I can to raise money and awareness for both the epilepsy and mental health communities.

This Too Shall Pass: What It’s Like Working at a Nursing Home in a Pandemic
Growing up, whenever something bad happened or I was going through hard times, my grandmother used to say, “This too shall pass.” Born in 1917, she lived through the Great Depression and World War II. She once described her life as hard but good, and Grandma always turned to that phrase for hope, often sharing it with others. Though Grandma has been gone for several years, her memory and wisdom are never far from my thoughts.That was never more apparent than on November 30, 2020. My shift had ended, and I had clocked out. I was on my way out the back door of the nursing home, putting on my coat and grabbing my purse from my locker, when a coworker from the kitchen passed me by saying, “Hey, have you heard? Two of the residents have tested positive for COVID-19!” I froze in place, my heart began to palpitate and goosebumps rippled across my skin. “Dear God, no!” I whispered, part prayer and part exclamation.
The Virus Entered the Nursing Home and Protocols Changed
For the past nine months, I had been working as a housekeeper in a nursing home. The workload was heavy, and I initially feared I wouldn’t be able to keep up, due to inexperience and my struggles with anxiety and depression. But I soon found my place there and fell in love with the residents, forming close friendships.Almost simultaneously, COVID-19 came to America, and protocol in the nursing home changed. We went from being barefaced to wearing cloth masks, then paper masks, then finally N95s and face shields. Plastic gowns were worn in isolation rooms and had to be donned and doffed for each new room. Six feet of distance was encouraged but couldn’t be followed because caring for the elderly requires close proximity. Every surface and high-traffic area had to be cleaned repeatedly. Various employees marched down the halls with sanitizer guns, blasting the railings and doors free of germs. But despite all of our attempts to protect the residents, COVID-19 had arrived at our facility. It didn’t take us long to figure out how the virus got in. An employee came in sick. None of that could be helped; COVID-19 could be asymptomatic and rapid tests often came back negative when someone was in fact positive. But this particular employee, and many others, neglected to wear their mask properly, allowing it to droop beneath the chin, and didn’t wear a face shield as instructed. I went home terrified. I had originally sworn that if the virus cropped up at the nursing home, I’d quit. I didn’t want to chance contracting it and bringing it home to my mother. But when I told my mother that two residents had been diagnosed with the virus, she wasn’t frightened. “You have to do what you’re comfortable with,” she responded to my news.

One of the ladies I cared about was not going to make it and her family wouldn’t be allowed into the unit to say their goodbyes.
I Began Working in the COVID Units and Braced for the Worst
I thought and prayed about it and came to the conclusion that COVID-19 was so widespread, and I could catch it anywhere. At least at the nursing home, there would be regular testing and PPE. In the end, my love for the residents won out, and I returned to work the next day. By then, seven residents were sick. First, the fire doors in the wing of the COVID unit were shut, but the hall rapidly overflowed with patients. Maintenance began to construct a new wall, consisting of a wooden frame and plastic sheeting—a surreal sight, it gave us chills as we watched it erected. Then, so many fell ill that a second wing was quartered off. My boss, the other housekeepers and I gathered around a table and went over the plans, and we were informed that housekeeping would have to go into the COVID-19 units every few days to clean. Originally, we had been promised that if the virus ever came to the nursing home, we would not have to go back into the unit. But requirements changed, and we would take turns going in. My turn came that Friday. “One of the COVID units needs to be cleaned. Are you willing to do it?” my boss asked. I nodded. “I’ll try.” My fear was that I’d end up in the fetal position, emotionally shaken by an anxiety attack.I gathered my supplies and went in. I was wearing a mask, face shield and a vinyl green gown, but it didn’t seem like enough to protect me. I cleaned anything and everything I could. A handful of residents were unaffected by COVID-19, displaying no symptoms, and they continued on with their routines the best they could. Others lay miserable and sweaty, wracked with a fever, hooked up to IVs and oxygen, unable to talk or recognize their surroundings, giving blank stares. The COVID stare. A chorus of violent coughs bombarded me at every turn. They hadn’t been bathed in days, too weak to leave the beds. Stink permeated the air. One man kept stripping himself, unable to bear the fever and, at one point, ripped his IV out. The first time in the unit was the hardest. I worried that every breath I took I was inhaling the virus. But the residents, those doing well and those suffering, faced it bravely and didn’t let it deter them. Their courage and strength emboldened me to return a number of times.
One man kept stripping himself, unable to bear the fever and, at one point, ripped his IV out.
It Was Painful to Say Goodbye to Patients During the Holiday Season
Weeks passed and the writing was on the wall: One of the ladies I cared about was not going to make it and her family wouldn’t be allowed into the unit to say their goodbyes. She was hooked up to an IV and oxygen, a sure sign she was slipping away. While I was there to clean, I was able to briefly hold her hand. “Hey, it’s me, your pal.” I sighed, brokenhearted at the sight of her detached from reality. She had one foot in this world and one in the next. “I’m going to miss you, but it’s going to be OK. I love you, and I’ll never forget you. See you later.” She died the next day, one of ten residents who passed away. No one should have to die alone, especially during the holidays. As Christmas neared, all I could think about was what an awful holiday season it was. For the residents, for those who lost loved ones and for myself too. I was in a bad place, and though I went home every day, it was impossible to shake off what happened at the nursing home. On December 21, there was a rare conjunction of Jupiter and Saturn, forming what was called the Bethlehem star. That night, Mom and I went outside to our backyard to try and find it. We saw a bright little flicker, brighter than the other stars, and believed we found it. I took it as a sign, a beacon of hope, and remembered what my grandmother used to say. “This too shall pass,” said the still, small voice from above. Somehow, some way, this pandemic would end. Not in December, or the next month, but someday.By January 2021, the outbreak at the nursing home was over, and my heart overflowed with joy as, one by one, the remaining residents left the COVID-19 units and returned to their rooms. Once more, life at the facility returned with a sense of normalcy. Residents went back to their routines and lived as they pleased. They were fairly unfazed by what they went through. That generation—my grandmother’s generation—refuses to be broken by hardship.I, on the other hand, will never forget the outbreak and will be forever marked by it. The virus and its effects will continue to haunt me. But my grandmother’s wise advice rings as true today as when she used to say it: This too shall pass. It offers me hope.


Sheer Willpower: How My Health Transformation Changed My Life
My most recent journey on the pathway to sound physical health all started on a seemingly normal Tuesday afternoon in February. After returning home from lunch with a friend, my wife announced what was to be the most liberating moment of my life: her intention to divorce me. (As a side note, her motivation to initiate the divorce was poor communication, incompatibility and basically “getting on each other’s last nerve.”) At the time, I was truly devastated and felt like a failure who was about to lose regular contact with my now 16-year-old daughter. During the last years of my marriage, I had slowly gained weight and approached 200 pounds. Laden with guilt and shame, I decided to embark on a path where I made the best of a stressful situation. My energy levels were low, and I felt sluggish from being overweight, so I silently concluded that I needed to revamp my entire lifestyle to improve my health. My chief motivating factor at the time was to reinvent myself in order to revitalize my relationships with my daughter and immediate family. My existence was fraught with grief, guilt and a sense of failure and impending loss. Physically, I was an absolute wreck. Thus, I chose not to feel even worse through a poor diet. Almost immediately, I cut my portion sizes, had lighter dinners, ate more fresh vegetables and reduced my intake of sweets and carbohydrates. By the time I moved out of the house, my weight dropped about 20 pounds from dietary adjustments alone. My divorce would be a blessing in disguise.
My divorce would be a blessing in disguise.
I Started a Workout Regimen and Saw Immediate Results
As my confidence grew and stress levels abated after the dissolution of my marriage that March, I redoubled my commitment to a healthier lifestyle. As soon as I moved from Boca Raton to Coral Springs, Florida, I joined Planet Fitness and quickly adjusted my schedule to work out as much as I could. By the summer, thanks to a workout regimen that required exercising four times a week and a diet consisting of proteins, fresh vegetables, low-fat milk and fruit, I dropped at least 20 pounds. My cardiologist and primary care physician were stunned (and impressed) by my transformation. Blood pressure and EKG readings, along with my lab results, showed vast improvements in my LDL, HDL, blood sugar counts and triglyceride levels. Once I saw the fruits of my labor (defined muscles, flatter stomach, chiseled face and so on), my sense of pride and confidence started to radiate in my personality, mood and attire. Honestly, I’m embarrassed to admit that I often posed in front of my mirror, flexing my biceps and looking at my flat stomach. My self-worth grew now that I was a freer, healthier and happier man. While looking at myself in the mirror, I immediately felt a rush of confidence and a sense of great achievement that would ultimately save my life. As a result of my new outlook on life, renewed health and slow self-discovery, I started to date women by the end of summer. Instead of looking down at the ground in defeat (as was the case in my marriage), I walked with a confident gait, head always held high. Women took note of this, and since my divorce, I’ve been involved in three serious relationships (including my current one). Two of the three partners were impressed with my commitment to leading an active lifestyle and one even referred to my fit body as “my trophy.” Such observations further motivated me to stay the course of healthy eating and exercise. My current romantic partner is a devotee of healthy, natural living and fitness. This characteristic is certainly another major motivating factor for my continued pursuit of a health- and fitness-oriented lifestyle.

The nasal orchestra was retired.
My Health Conditions and Family Life Have Improved Drastically
Of course, there were other positive effects from leading a healthy lifestyle. While engaged in passionate political or personal conversations, I’m no longer gasping for air because of being overweight. This has already enhanced my politically-oriented YouTube channel, which has earned a few hundred subscribers after existing for a few months. And, as a result of my enhanced physical energy, I’ve been able to perform my job functions with extra zeal. Even my overall sleeping patterns have improved and I no longer snore like a tuba or need a CPAP machine. Clearly, I ceased being an annoyance to any woman sleeping by my side. The nasal orchestra was retired. As I reflect on the two and a half years of my mental and physical revitalization, I am clearly satisfied with the trajectory of my life. My dramatic weight loss, improved blood count levels and other physiological changes benefitted me during this new phase. As I mentioned previously, my renewed physical energy and mental peace paved the way for a vastly improved relationship with my daughter and the rest of my family. It is my contention that a revived physical/physiological chemistry leads to clearer thinking, which in turn leads to sound decision-making and vastly increased self-confidence. Before my dramatic weight loss and improved blood chemistry/blood sugar levels, I felt sluggish and tired. This condition impeded my thought process and my self-confidence declined precipitously over the years. Such a mental state trickled down and affected my relationships with my daughter and family. My lethargy could be compared to the post-1977 United States or the late Western Roman Empire, which were arguably governments and societies in steady decline. They became too focused on satiation and trapped in materialism without any consideration for the long-term survival of their respective nation-states. As my life was slowly crashing around me, I experienced the equivalent of two Pearl Harbor situations (divorce and a near heart attack) and made a radical course correction.I can not only express pride in my accomplishments, but encourage others struggling with heart disease and weight loss with the hope they will stick to regimens that improve their lives.

My Husband and I Went on a COVID Coke Binge
I’ve always been open-minded and eager to try things outside the norm. Part of that comes from growing up with young, carefree parents, but the main reason is simply being queer in a world that isn’t catered for people like me. Going through shit, as many of us have, you learn to look below the surface rather than at what’s presented at face value. You actively oppose society’s stuffy expectations because a lot of the time, they don’t include you anyway.
I Was Born to Be a Cokehead
I wanted to try cocaine as soon as I heard about it, around age 19. I was about to leave the small city I grew up in to go to university in a larger one, and despite not knowing about the drug’s effects or repercussions, it sounded like the perfect introduction to my new life as a man of the world. Plus, I knew my parents had experimented in the past. It sounded like they had a blast.A week after starting university, I took cocaine with some new friends, and over the next few years, it became a weekly habit. The rush I got from coke was exhilarating, but what really drew me in was how confident and vocal it made me. As someone who had always been shy, it was as though for those brief periods of time, I could leap out of the cocoon of my old self and become the butterfly I saw as my ultimate incarnation.Fifteen years later, my carefree attitude has mellowed somewhat—but not entirely. I got married last year, and as I’ve grown older and surer of myself, my confidence has grown without the help of performance-enhancing drugs. Over the course of my 20s, coke went from a once a weekend staple to a special treat I gave myself once or twice a year.Until the pandemic started.

The sudden lack of structure, so much like my younger days, caused old ways to come hurtling back.
Lack of Structure Sent Me Out of Control
My husband and I both contracted COVID-19 during the U.K.’s first lockdown. He was bedridden, while I binged crap on Netflix and suffered through not being able to taste anything I ate. Thankfully, we both recovered and were fortunate enough to be furloughed from our jobs. But the sudden lack of structure, so much like my younger days, caused old ways to come hurtling back.My husband isn’t quite as experienced as me when it comes to cocaine, but he had participated on the rare occasions I had done it since university. But over the course of lockdown, sharing a couple of bottles of wine in the evening soon turned into, “Let’s just get on it; we don’t have to get up for anything tomorrow.” I got the number of a dealer from a friend, and soon, we were banging out a gram each week.When you’re high on cocaine, everything is amazing. You feel invincible, creative, ready for whatever’s around the corner. My husband and I grew closer those nights as we spoke about things we’d never dared to when we were sober, like having kids or our difficult sex life. We nearly even had a threesome, which in hindsight wouldn’t have been good for our relationship, on top of not being very COVID-safe. We were living in our own little bubble, free of the worries and stress that the world outside ordinarily held for us.
Soon, we were banging out a gram each week.
I Just Can’t Get Enough
My husband, and those I’ve done cocaine with in the past, knows when enough is enough and it’s time to say farewell to a great night. I don’t. I must finish what’s left, even if it’s midday and I’m doing it solo, even if my chest is hurting and I can’t feel my heartbeat because of how fast it’s going. All I want is that next fix. Soon enough, our little quarantine treat blew up into a toxic cycle of weekly use—until we were forced to stop.During the summer, our furlough stopped. We lost our jobs, and, unsurprisingly, our money was running out. We could no longer afford to live where we were, so out of necessity, we decided to move in with a relative. It was far from the city we’d called home for years and away from the toxic, structureless bubble we’d created. I had no choice but to quit.By then, my health had started to deteriorate from how far we had taken our drug binges. Several blood vessels in my nose had popped, ravaging the exterior, and I regularly got shooting pains in my chest. Had moving saved me from damaging myself further—and possibly even saved my life? I think so.Now my health is back on track and my living situation is much more stable, and I can see that the hole I was in was more out of routine than anything else. When I do cocaine again—and when we next visit friends who do it, I will—I’m not worried that it’ll become a habit again. But I worry that other people who’ve fallen into similar toxic cycles during the pandemic won’t be so lucky.
